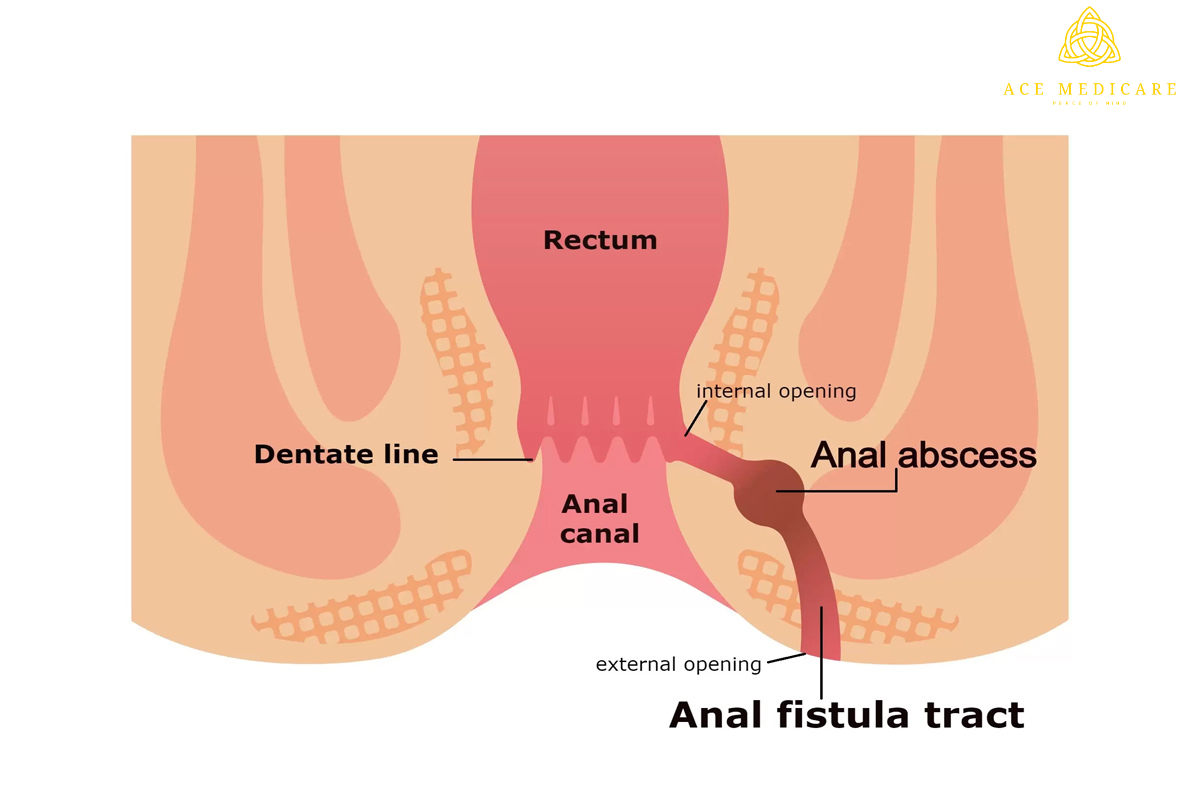
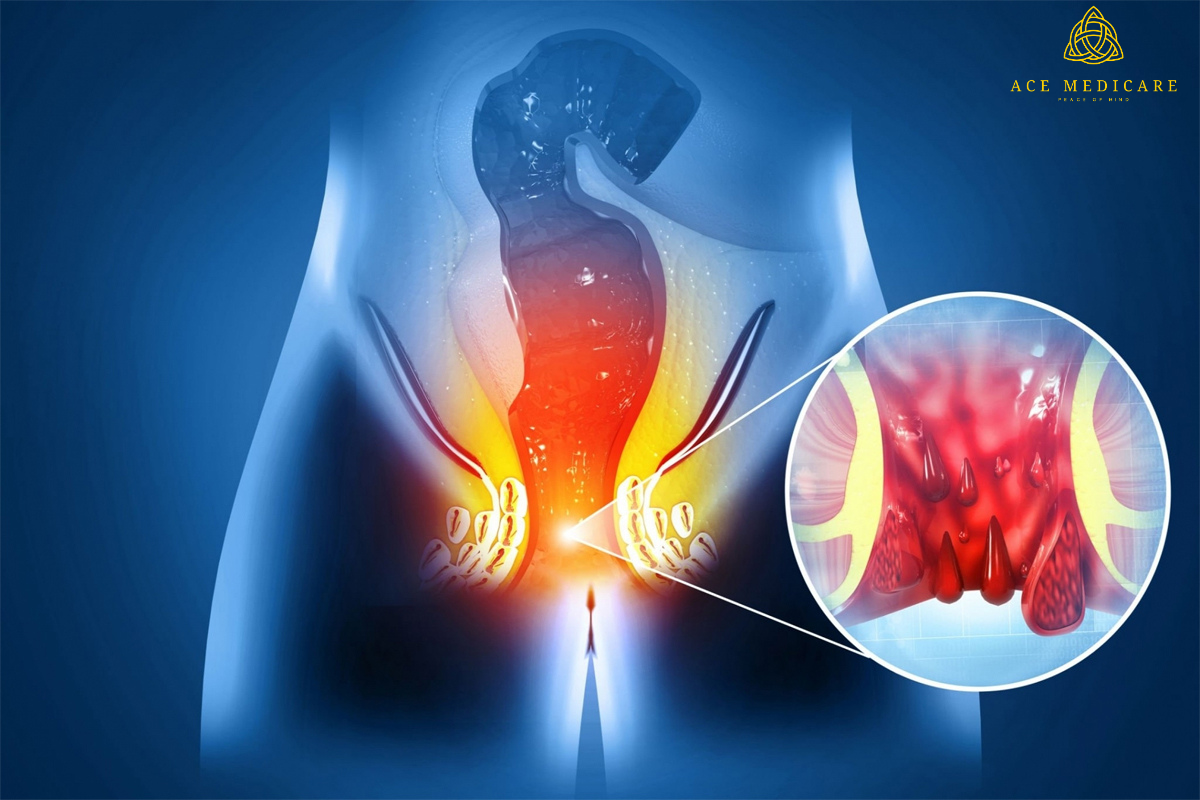
Exploring Surgical Interventions for Anal Fistula: A Comprehensive Guide
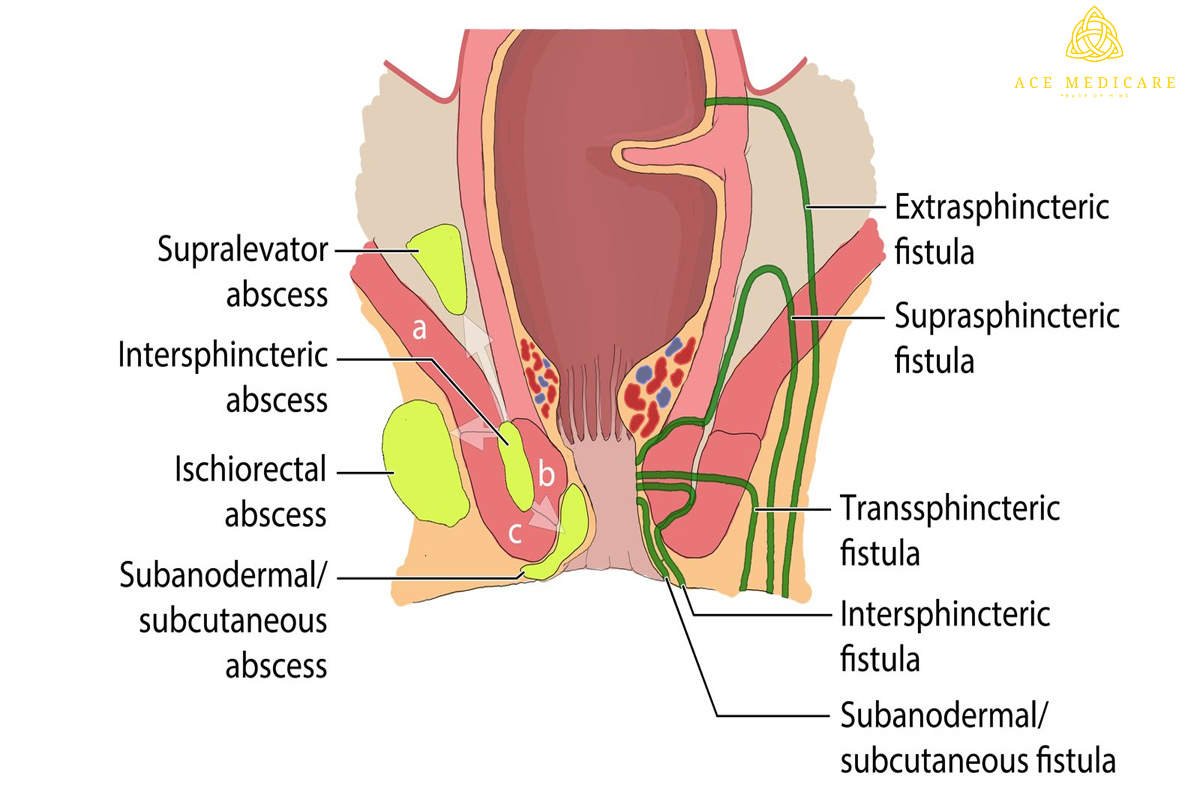
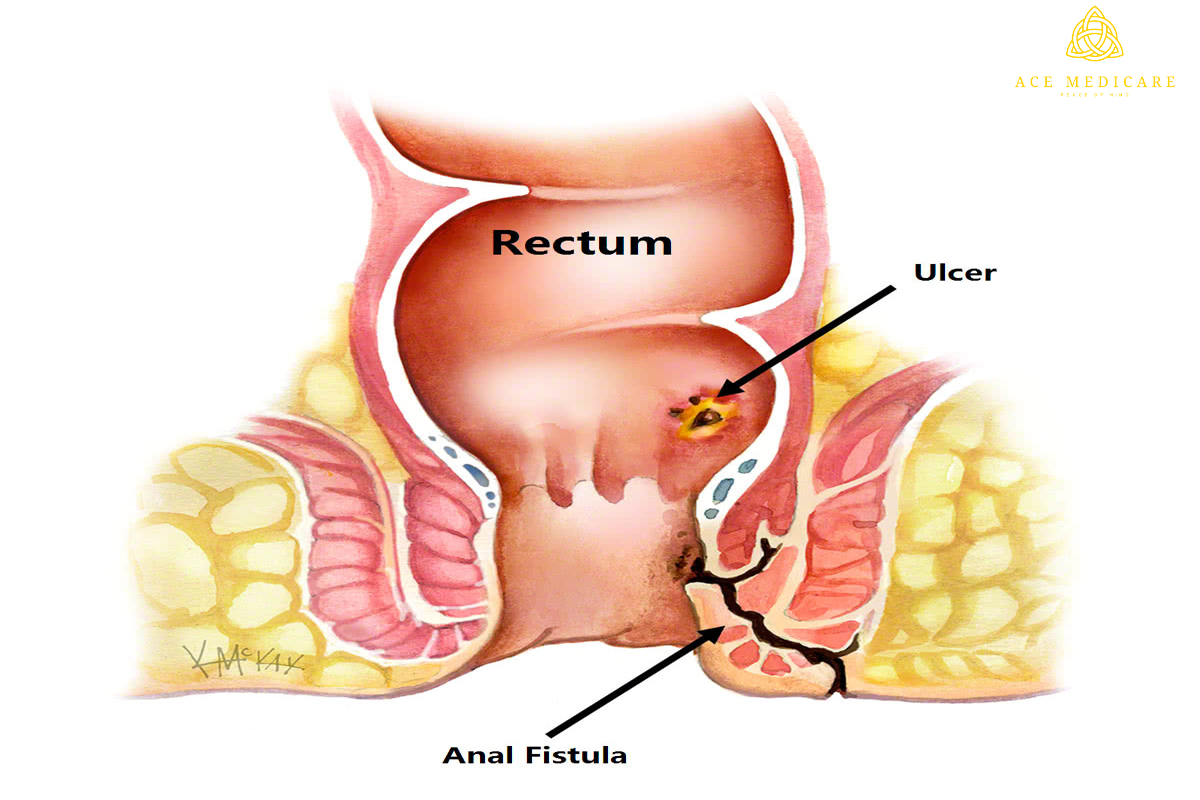
Introduction Fistula, an improper connection between two body parts, is a difficult medical problem that requires extensive understanding and care. Treatment options range from simple drugs to sophisticated operations, and are mostly determined by the type, size, and location of the fistula. This thorough handbook seeks to traverse the diverse world of fistula therapy, providing insights into both traditional and cutting-edge methods.
- Biologic Therapies: Anti-TNF drugs (e.g., infliximab, adalimumab) are used to treat fistulas associated with IBD, such as Crohn's disease. These medications reduce inflammation and promote healing by targeting specific proteins involved in the inflammatory process.
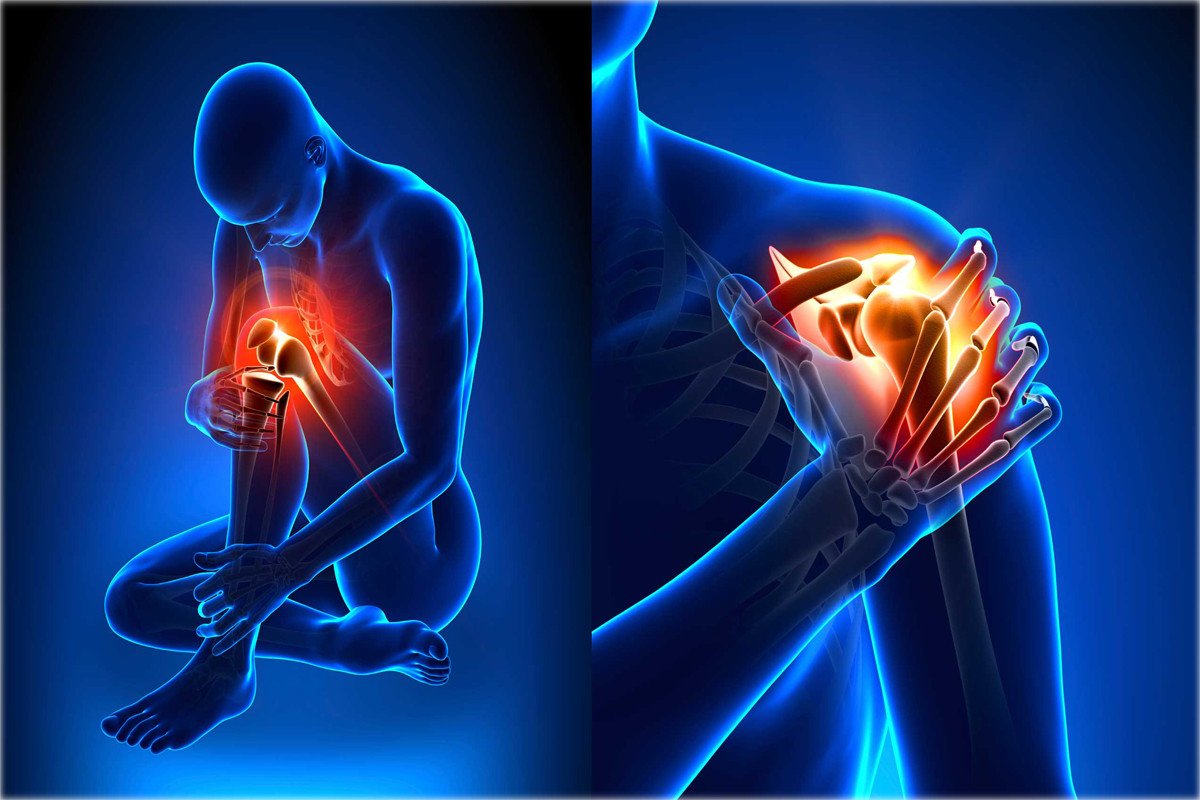
- Pain relievers: To address the pain and suffering caused by fistulas, pain medications such as nonsteroidal anti-inflammatory medicines (NSAIDs) or opioids may be administered.
- Biologics for Other Diseases: When fistulas are present,Adalimumab, which is related with conditions such as hidradenitis suppurativa, may be used to treat inflammation and prevent new fistula formation.
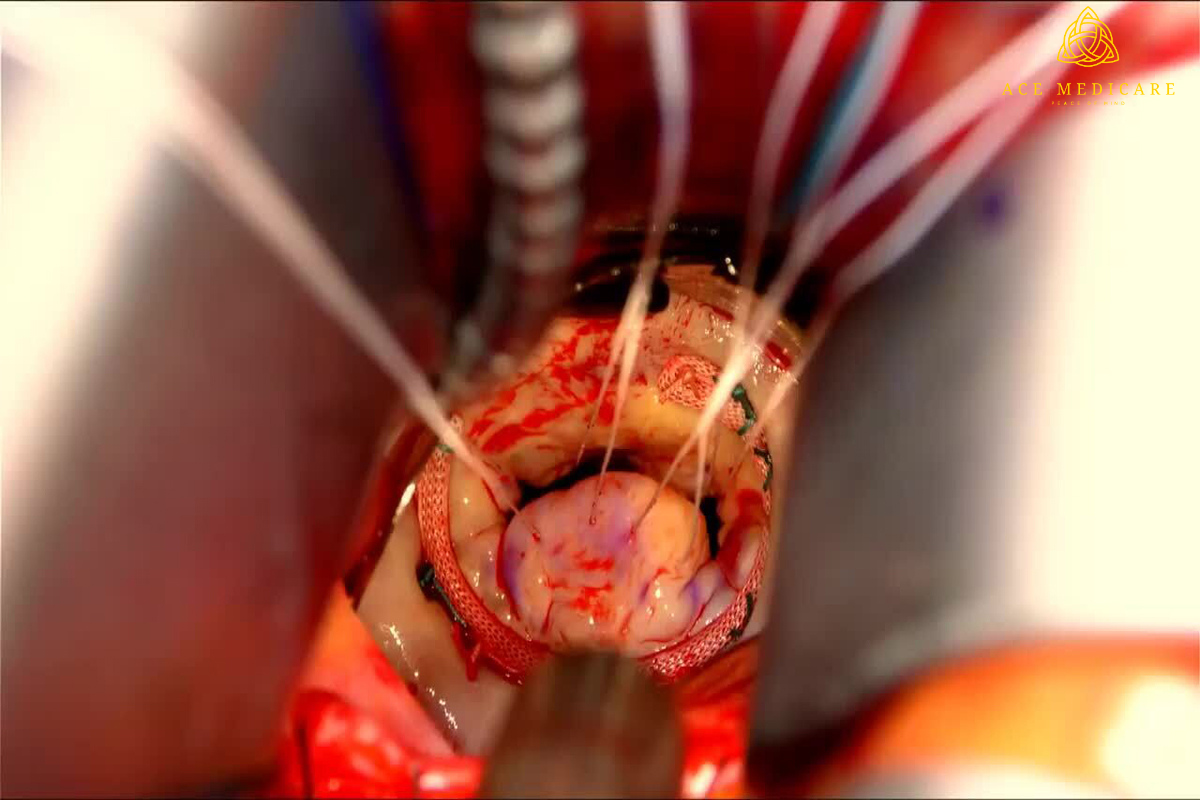
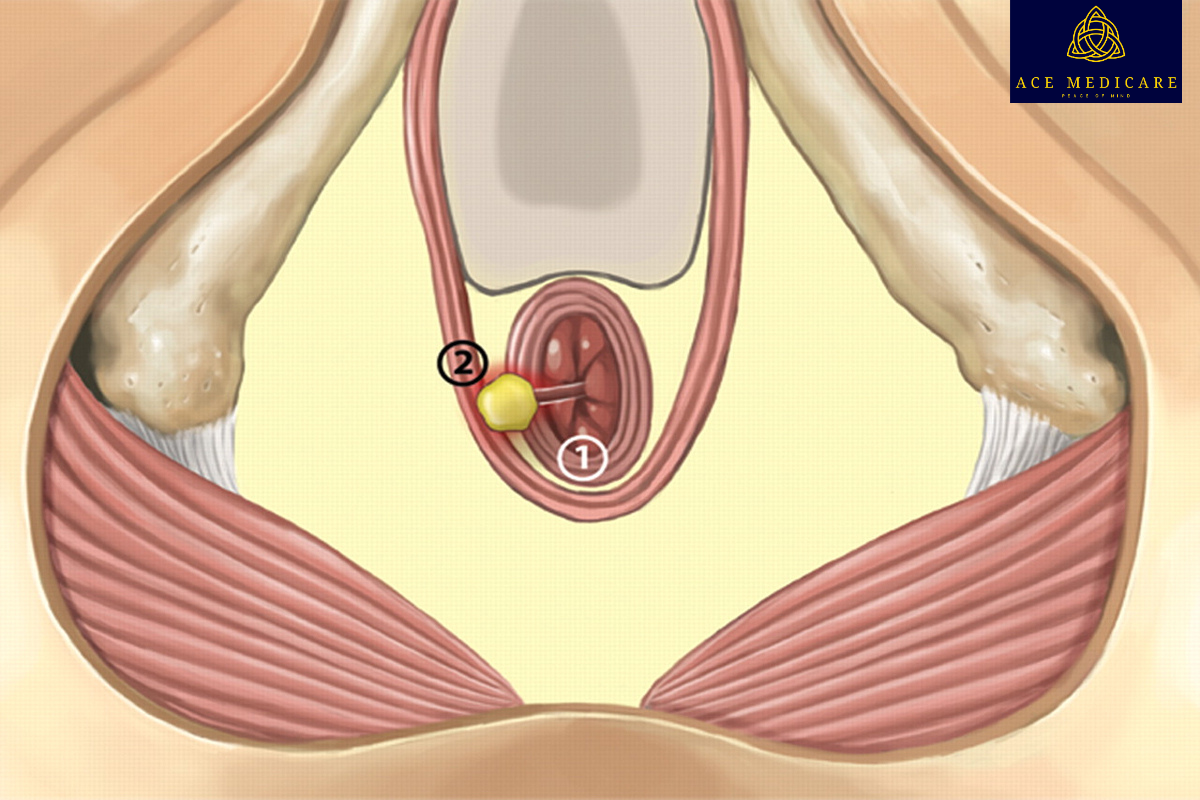
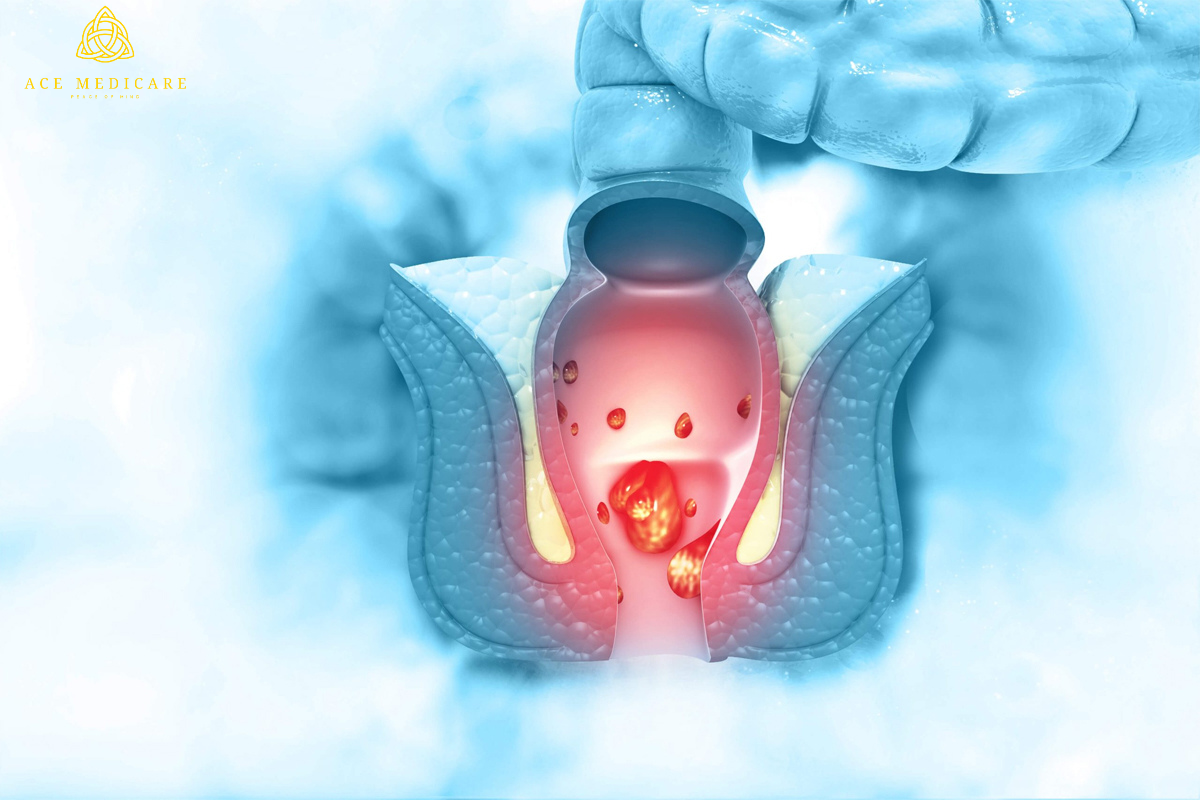
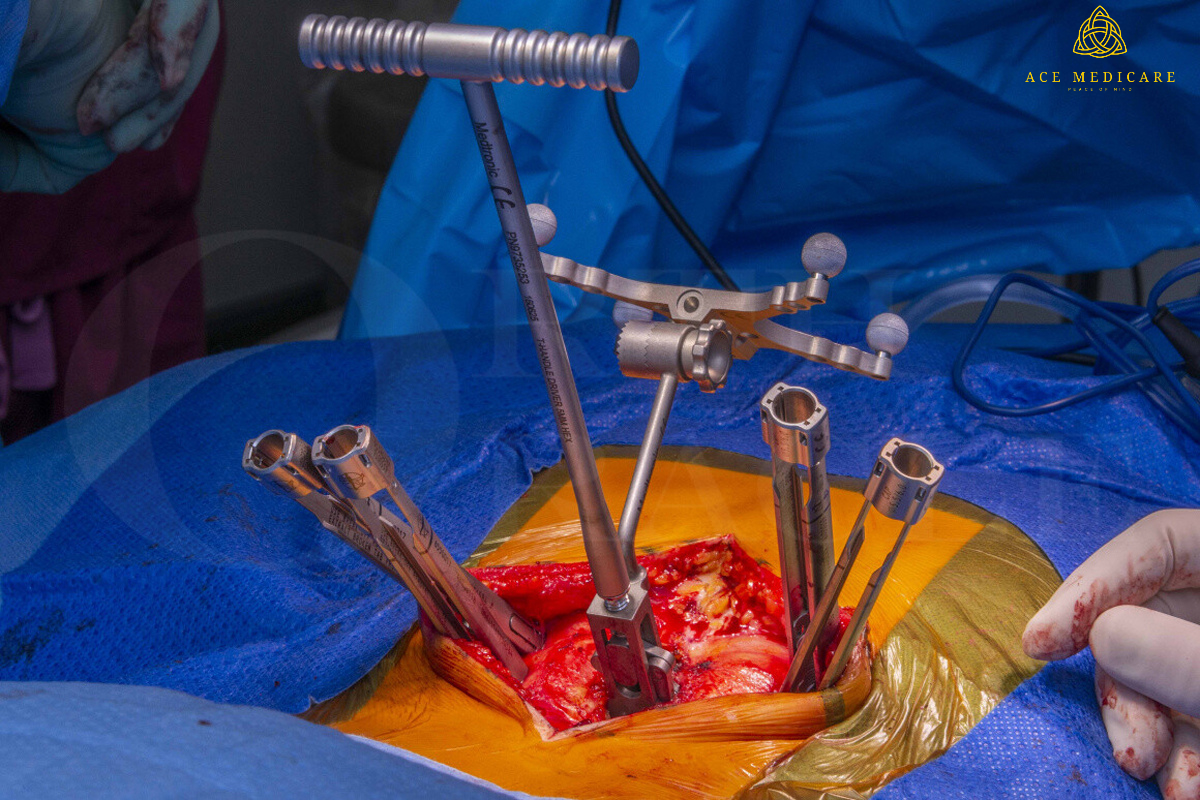
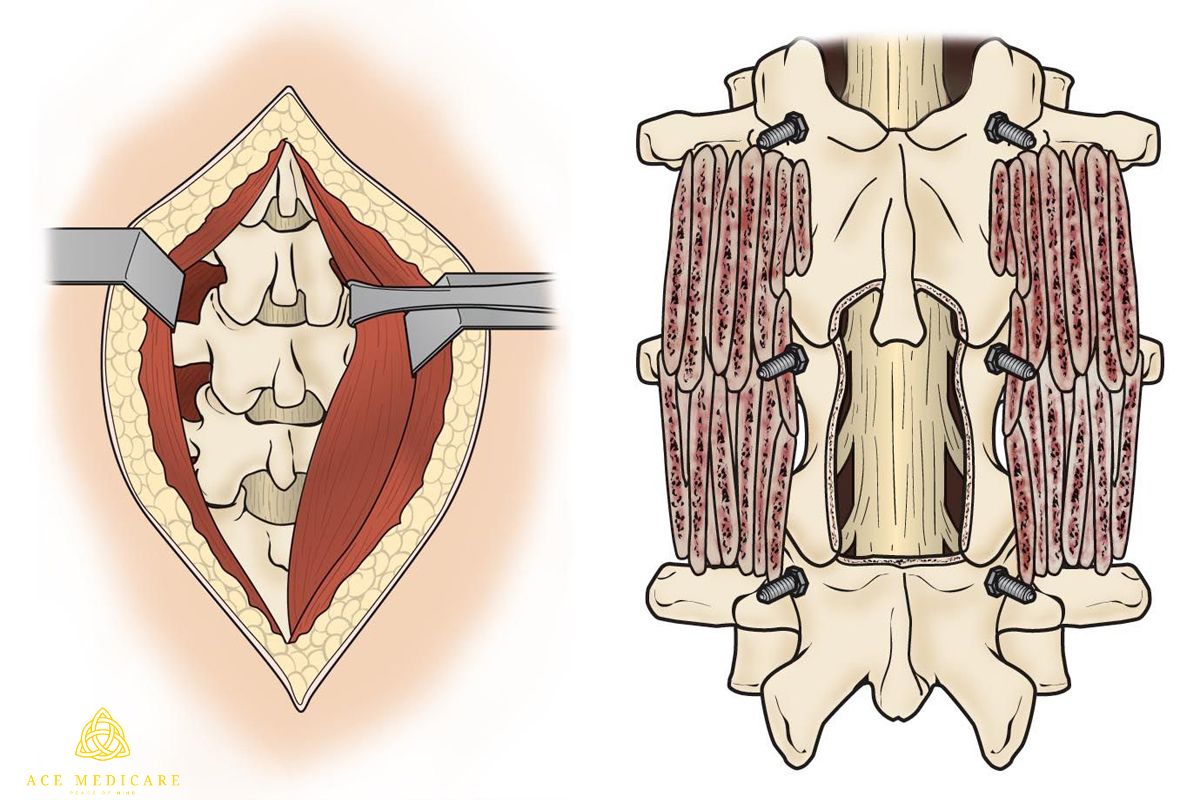
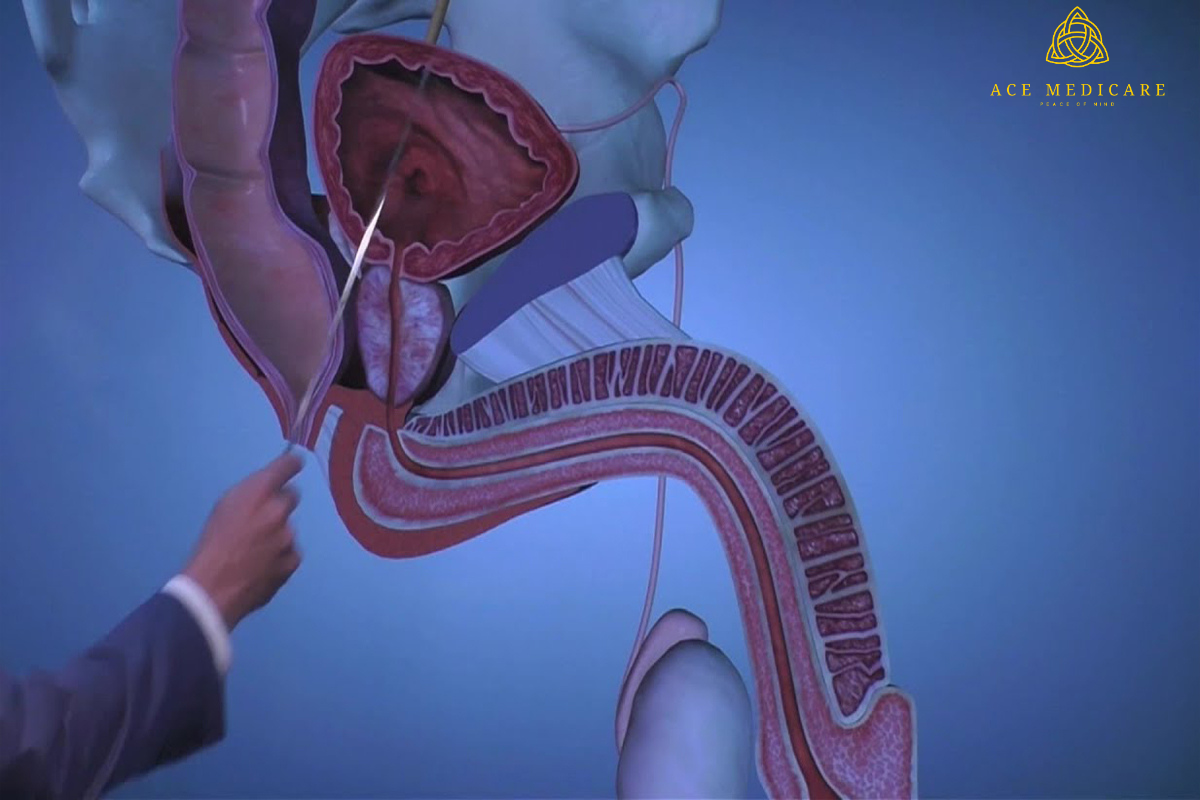
- Seton Placement: A seton is a piece of surgical thread or substance that is inserted through the fistula tract. This promotes drainage while progressively cutting down the tract to allow for eventual healing.
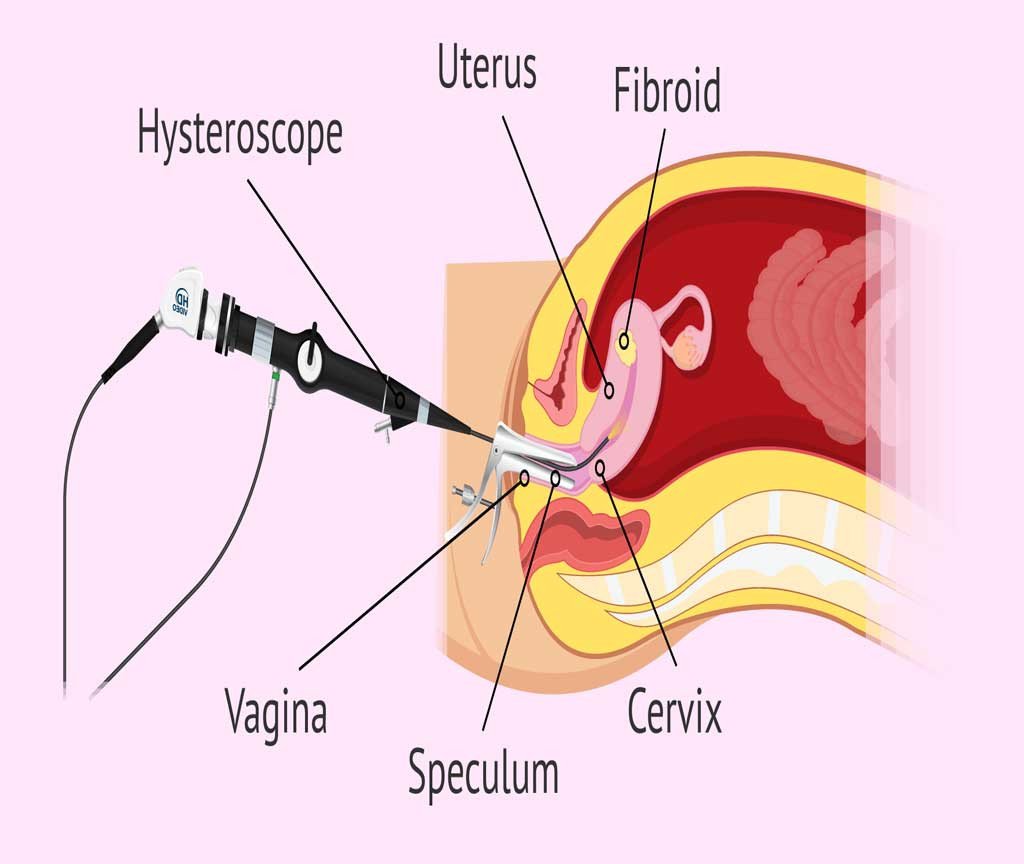
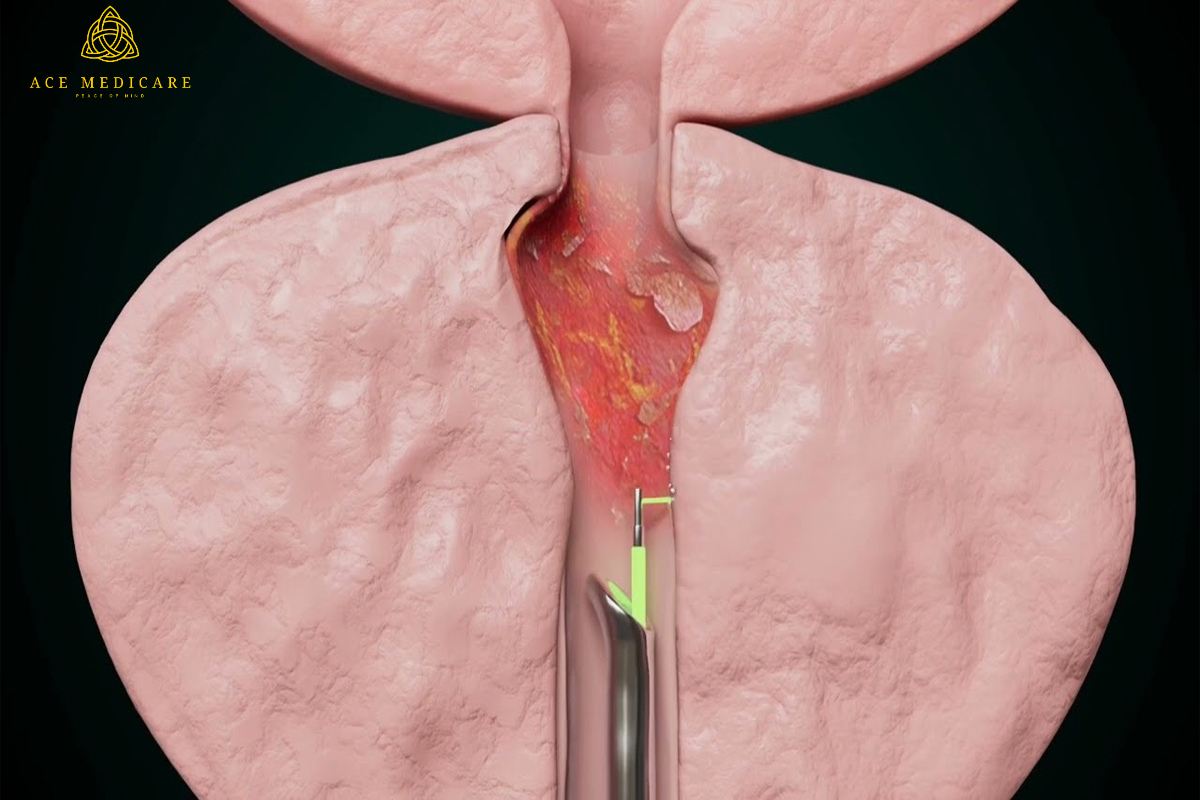
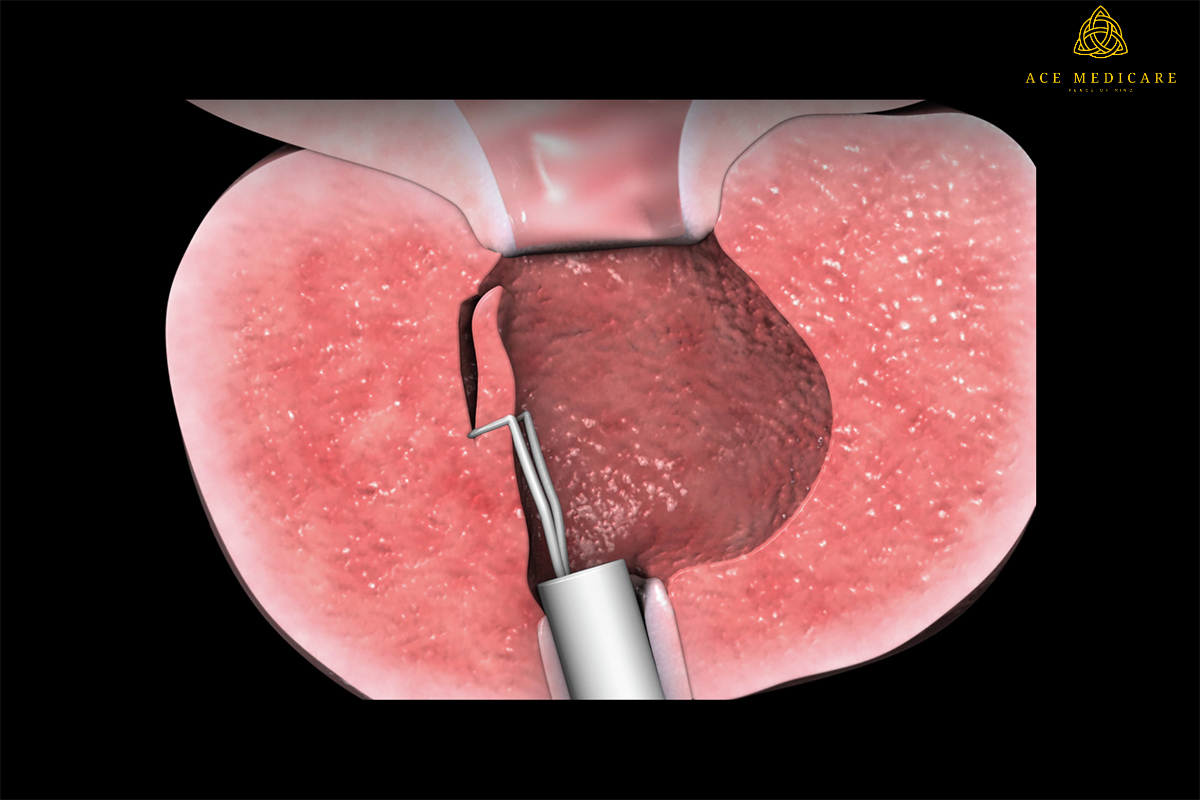
- VAAFT (Video-Assisted Anal Fistula Treatment): VAAFT is an endoscopic treatment for treating anal fistulas. To find and shut the internal opening, a camera-equipped endoscope is placed into the tract.
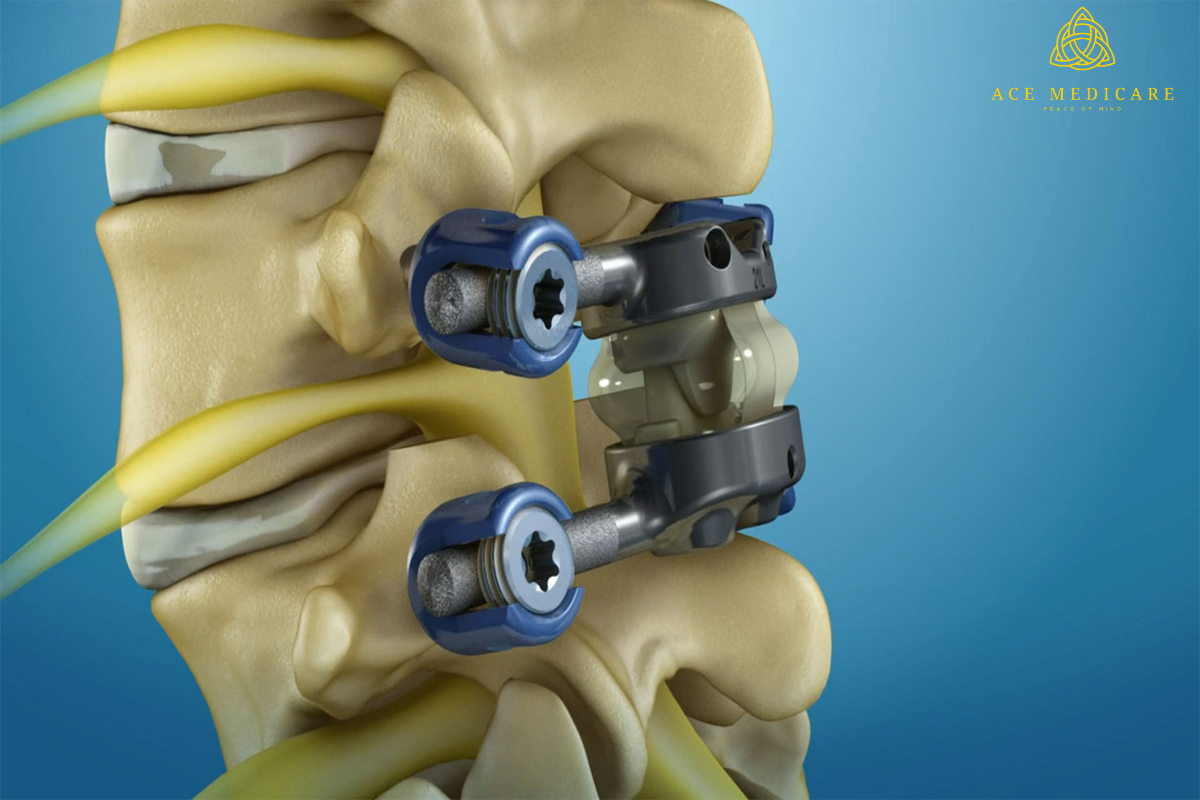
- LIFT (Ligation of the Intersphincteric Fistula Tract): LIFT ligates the tract to block the channel in high intersphincteric fistulas.
- Fibrin Glue Injection: To close some forms of fistulas, fibrin glue can be injected.
- Transanal Minimally Invasive Surgery (TAMIS): TAMIS uses specialised equipment and an endoscope to enter the fistula from within the rectum.
Minimally invasive approaches provide individualised solutions for different types and locations of fistulas, increasing patient outcomes and quality of life. A consultation with a professional is required to establish the best treatment for an individual's specific circumstance.
- Cleaning and Excision: The afflicted tissue and tracts are meticulously cleansed and excised, with any infected or damaged areas removed.
- Drainage: The wound is normally left open to allow for drainage and is not sutured closed. This open wound heals from within.
- Healing: The wound heals and the fistula disappears over time. The healing process could take many weeks, and it's critical to keep the area clean.During this time, keep your home clean and well-maintained.
- Minimally intrusive: When compared to standard surgery, this method is less intrusive, which frequently results in a faster recovery.
- Laser treatment has a lower chance of injuring the anal sphincter muscles, lowering the likelihood of incontinence, which is a major issue in fistula surgery.
- Lower Post-operative Pain: Post-operative pain and discomfort are often reduced in patients.
- Reduced Recurrence Rates: Although additional long-term evidence is needed, several studies suggest that laser treatment may have lower recurrence rates.
- Effectiveness: Depending on the type, size, and location of the fistula, the effectiveness may vary.
- Cost: Laser treatment can be more expensive than other types of treatment.
- Availability: This treatment may be available.be restricted to specific healthcare facilities or regions.
- Long-term effects: Additional research is required to completely comprehend the long-term effects and potential issues.
Attend all follow-up appointments so that your healthcare practitioner can monitor your healing process and address any issues.
- Medication Compliance: To prevent infection and manage discomfort, take all prescription drugs, including antibiotics and pain relievers, as advised.
- Wound Care: To improve healing, keep the surgery area clean and dry, and follow your healthcare provider's wound care instructions.
- Dietary Alterations: Adopt a high-fiber diet to promote regular bowel movements and avoid straining, which can impede healing.
- Hydration: Drink enough of fluids to keep your bowel movements regular and your general health in check.
- Avoid heavy lifting and other strenuous activities.vigorous activities as directed by your healthcare practitioner to avoid putting undue strain on the healing region.
- Sitz Baths: If advised, take sitz baths to soothe the area and improve recovery.
- Participate in physical therapy activities to strengthen pelvic floor muscles and enhance sphincter control if recommended.





.png)





.png)






.png)























.png)






































.png)























.png)
.png)





.png)































.png)




.png)





.png)












.png)






.png)