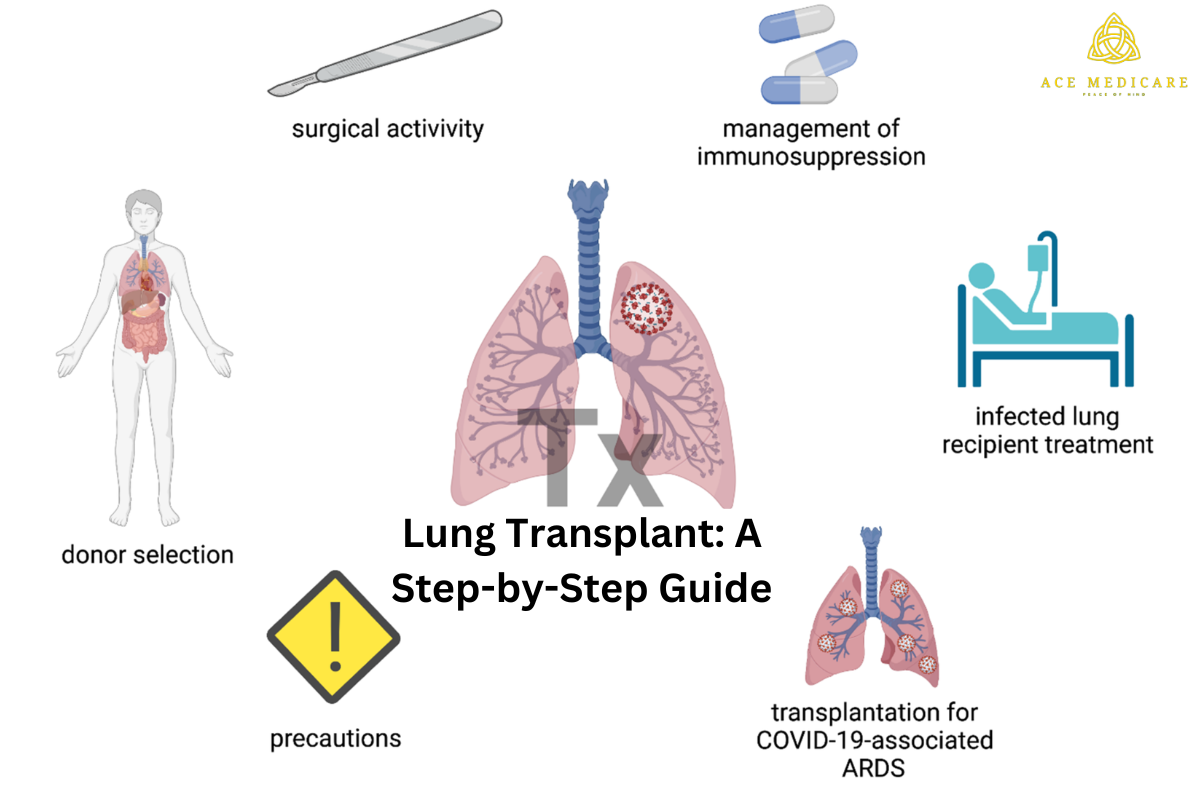
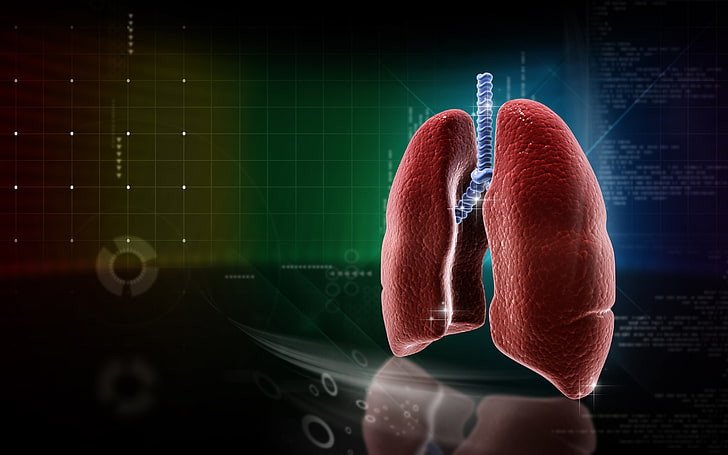
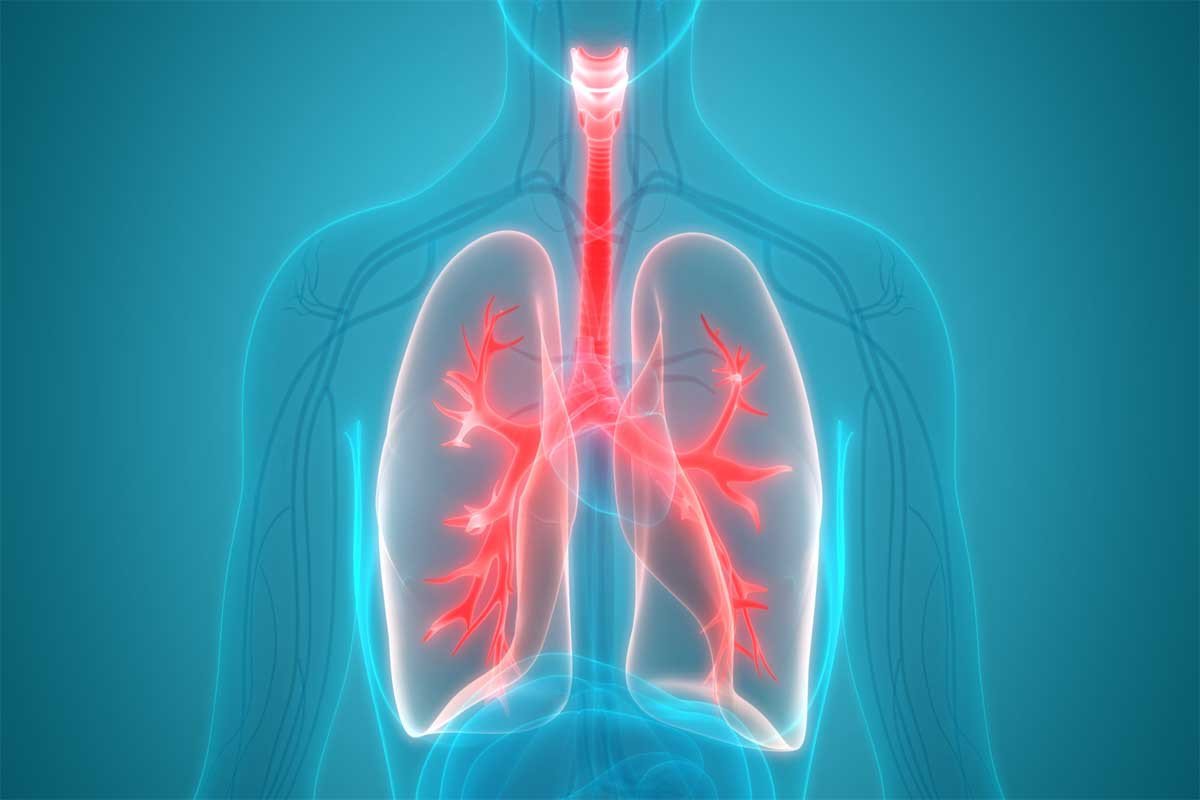
Lung Transplant: A Step-by-Step Guide
A lung transplant is an intricate medical procedure that serves as a beacon of hope for individuals grappling with severe lung diseases. This step-by-step guide by Ace Medicare aims to provide a comprehensive understanding of the entire process—from the conditions that may necessitate a lung transplant to the transformative impact it can have on the lives of recipients.
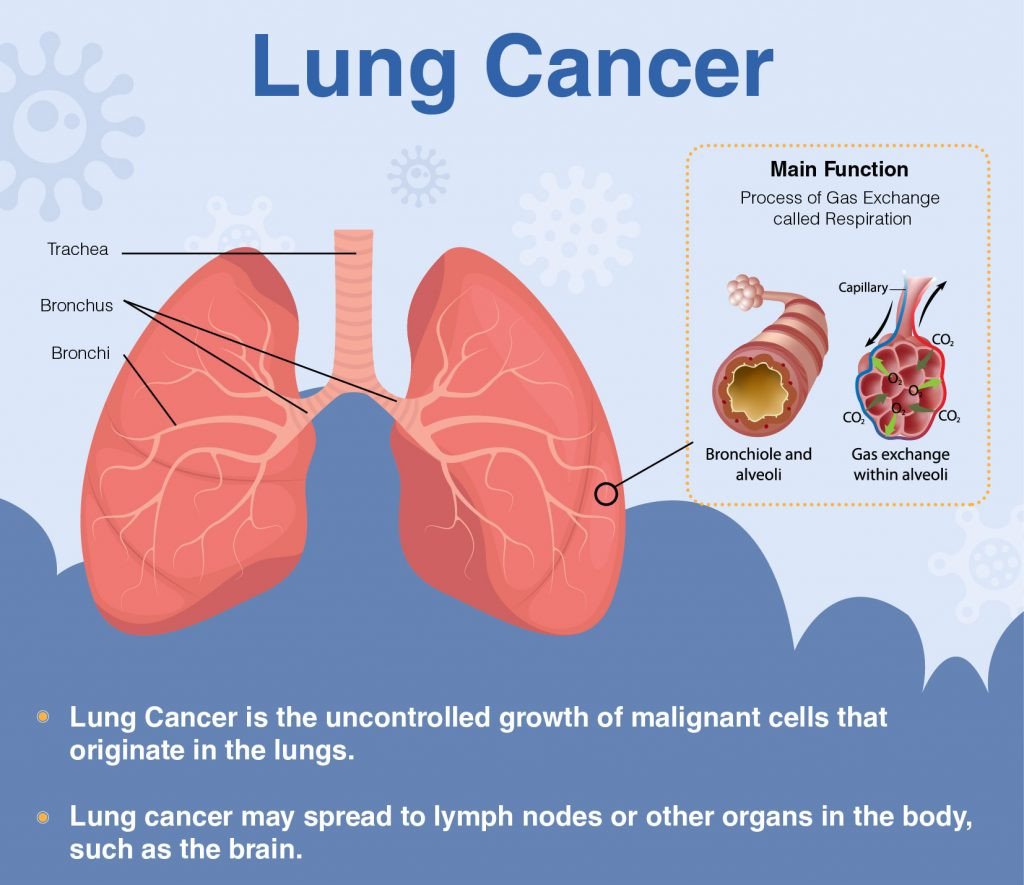
1. Understanding the Journey to End-Stage Lung Disease:
The journey toward a lung transplant often commences with the diagnosis of end-stage lung diseases such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis, or cystic fibrosis. As these conditions progress, individuals experience a profound decline in lung function, marking the beginning of the consideration for a lung transplant when other treatments become insufficient.
2. Evaluation and Eligibility: The First Steps:
Prospective lung transplant recipients undergo a rigorous evaluation process to determine their eligibility. This involves a comprehensive examination of medical history, lung function tests, imaging studies, and psychological assessments. The goal is to ensure that individuals are in suitable health to undergo the transplant procedure and manage the post-transplant challenges.
3. Types of Lung Transplants: Single and Double Lung Transplants:
There are two primary types of lung transplants—single lung transplant and double lung transplant. The choice depends on the nature of the recipient's lung disease. Single lung transplants are suitable for conditions like COPD, while double lung transplants are considered for diseases affecting both lungs, such as pulmonary fibrosis.
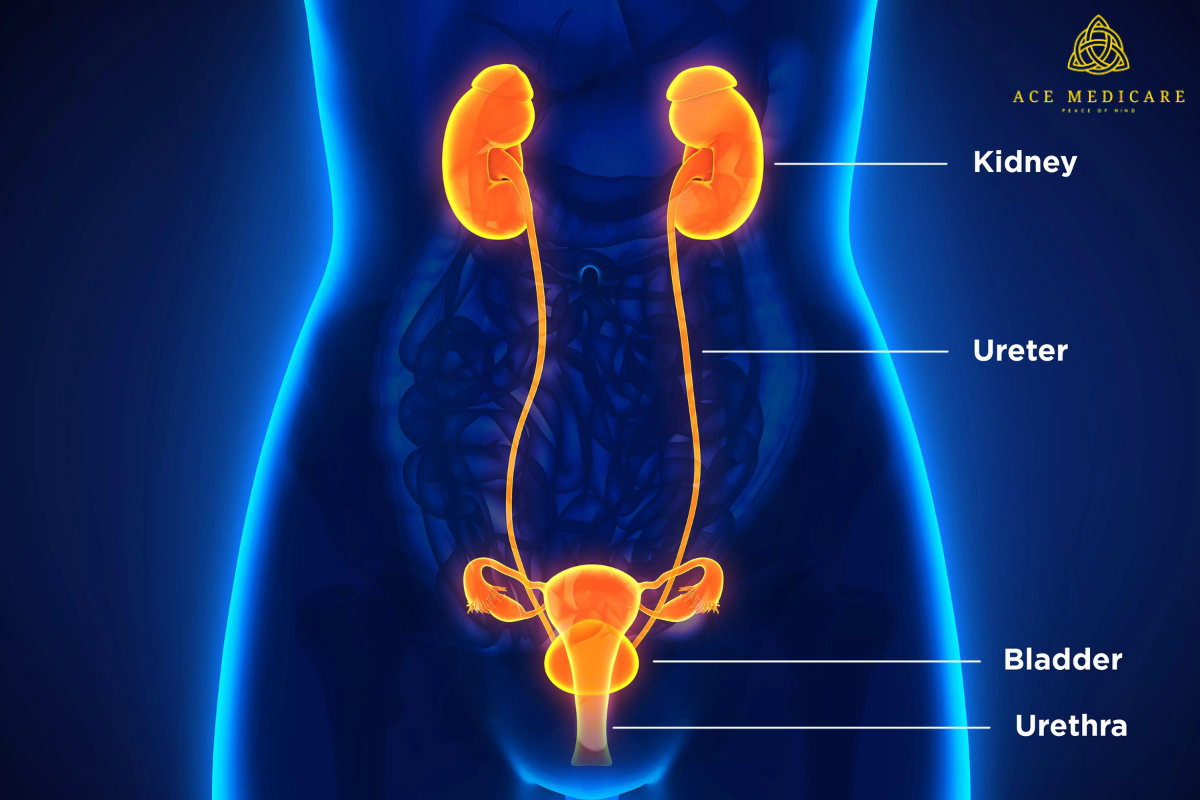
4. The Donor Matching Process: Piecing Together the Puzzle:
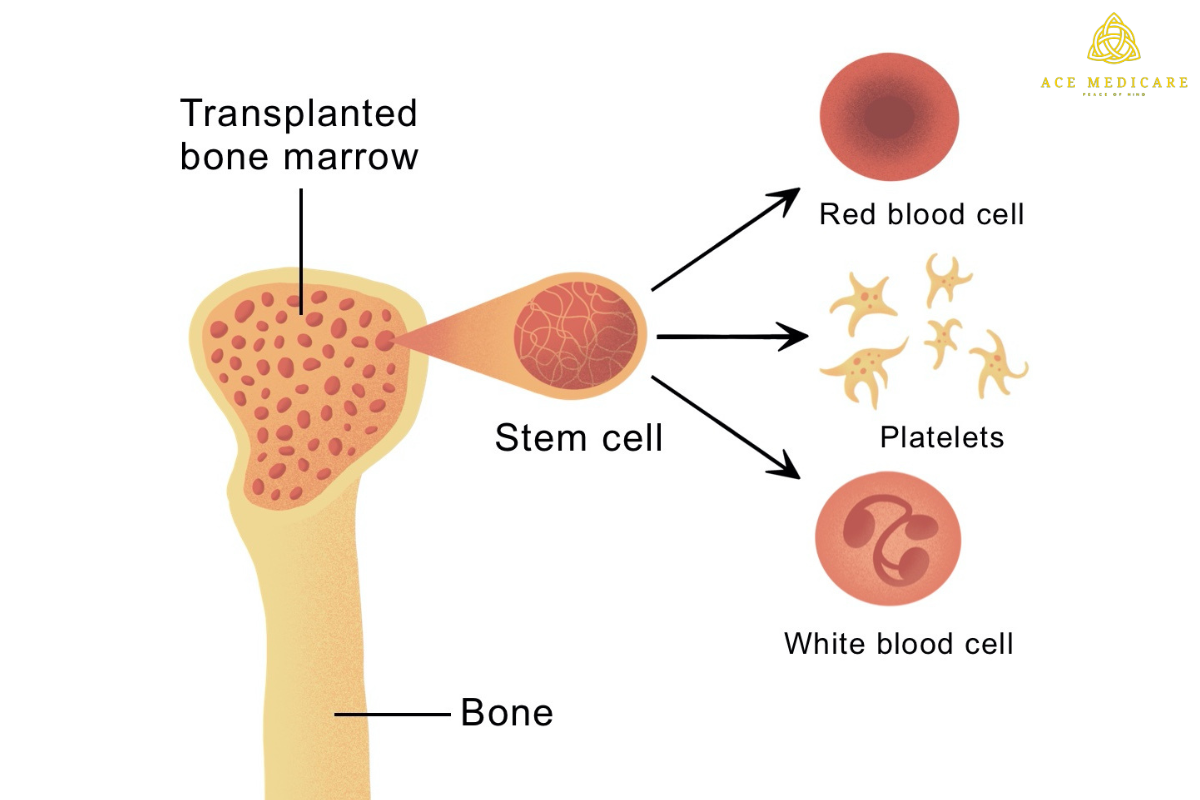
The success of a lung transplant hinges on finding a suitable donor. The matching process involves factors like blood type, tissue compatibility, and size matching. Urgency and geographical proximity also play roles in finding the right match. The donor matching process is a critical puzzle that needs meticulous attention.
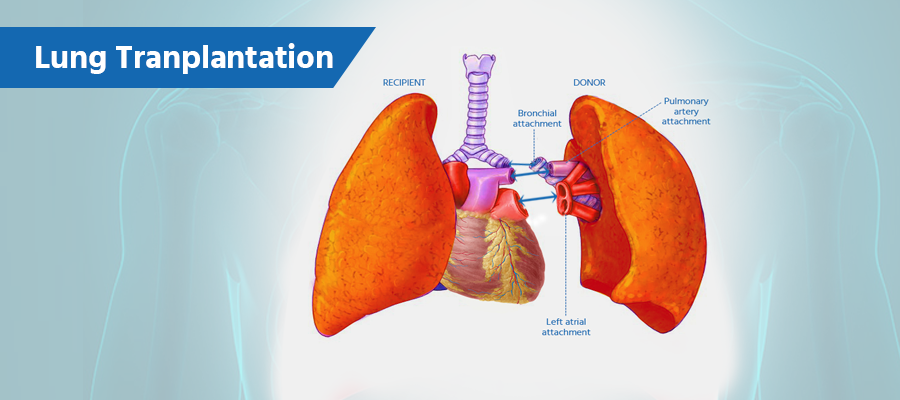
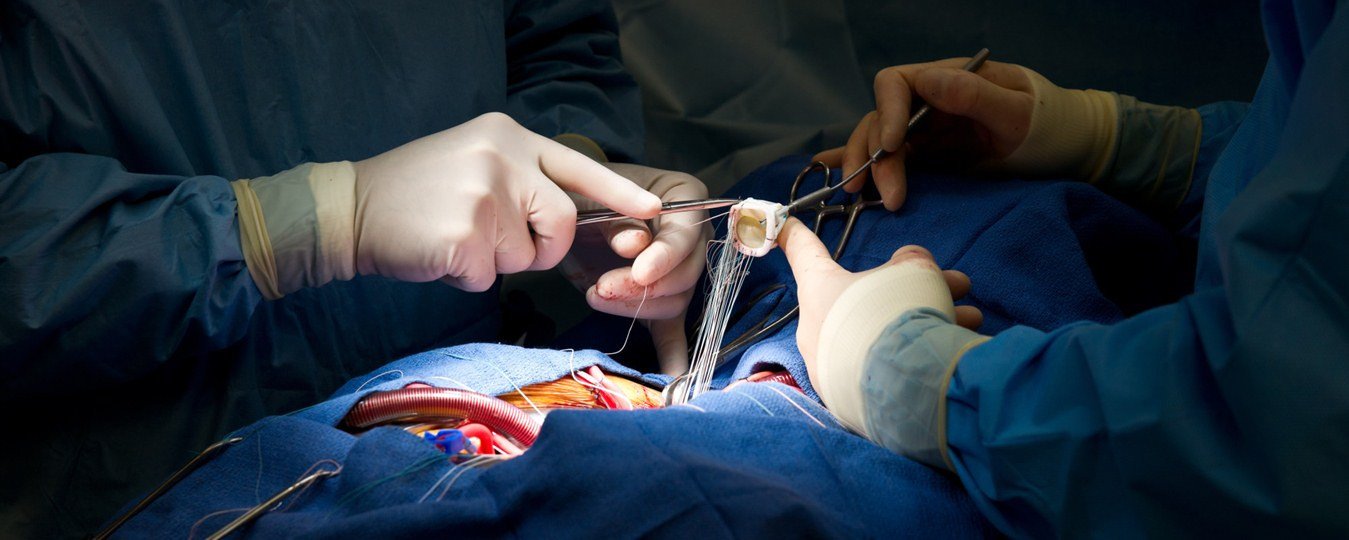
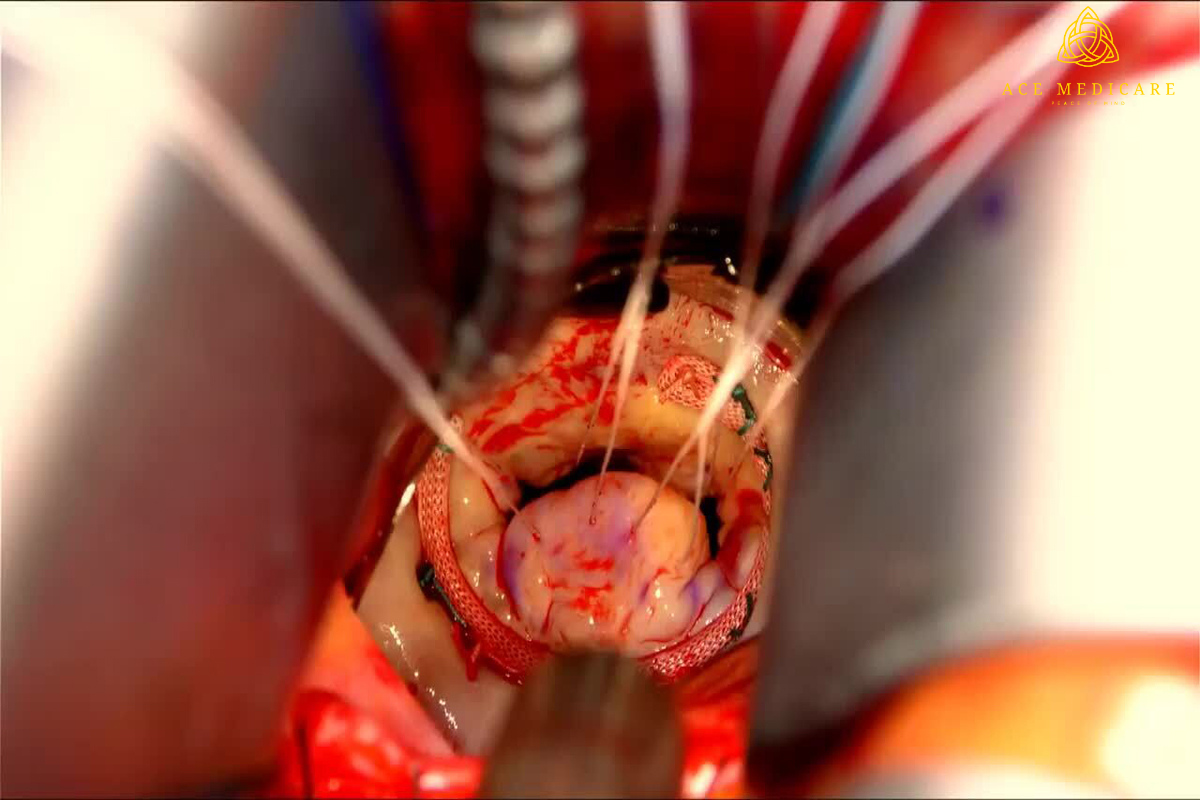
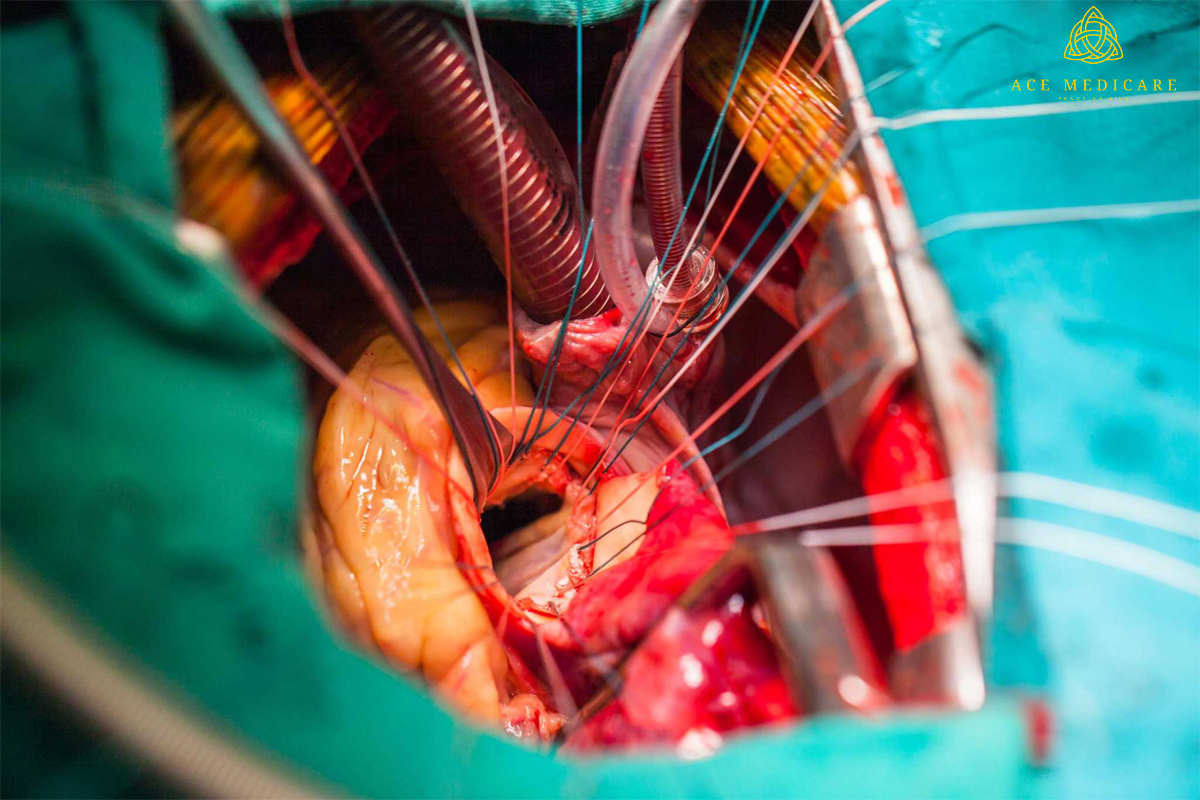
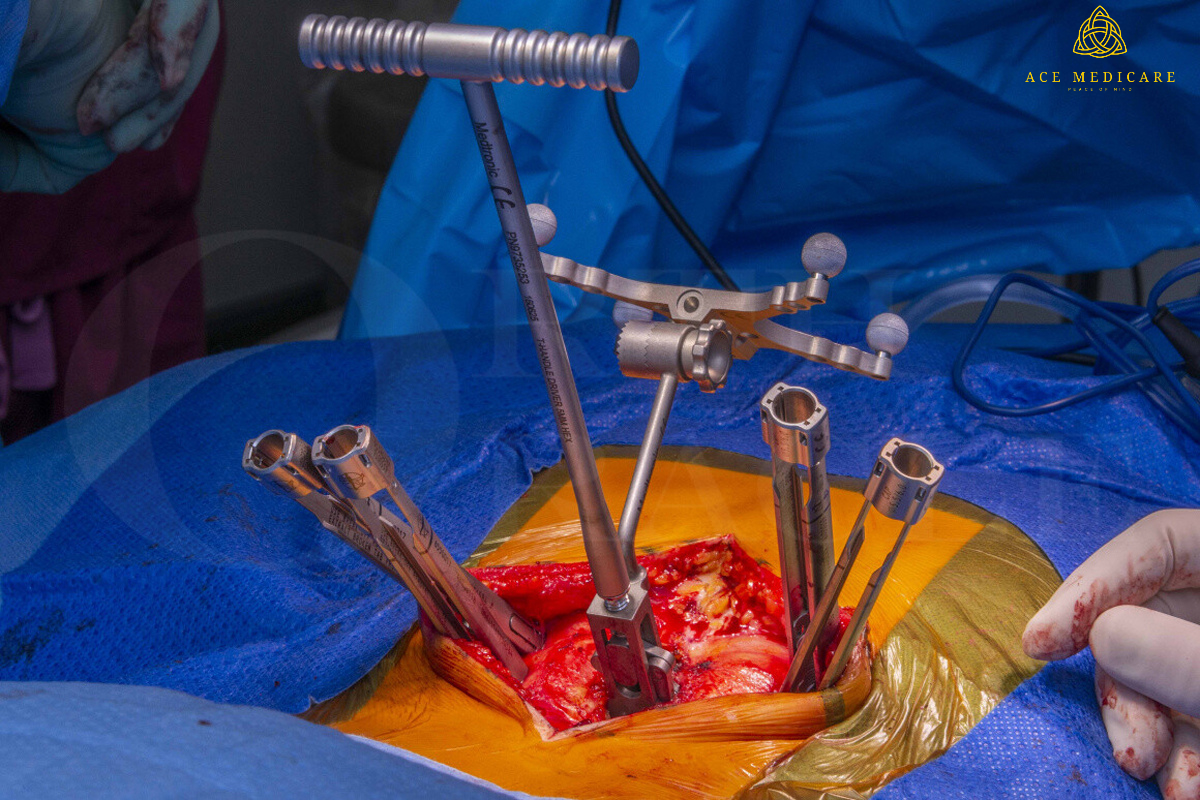
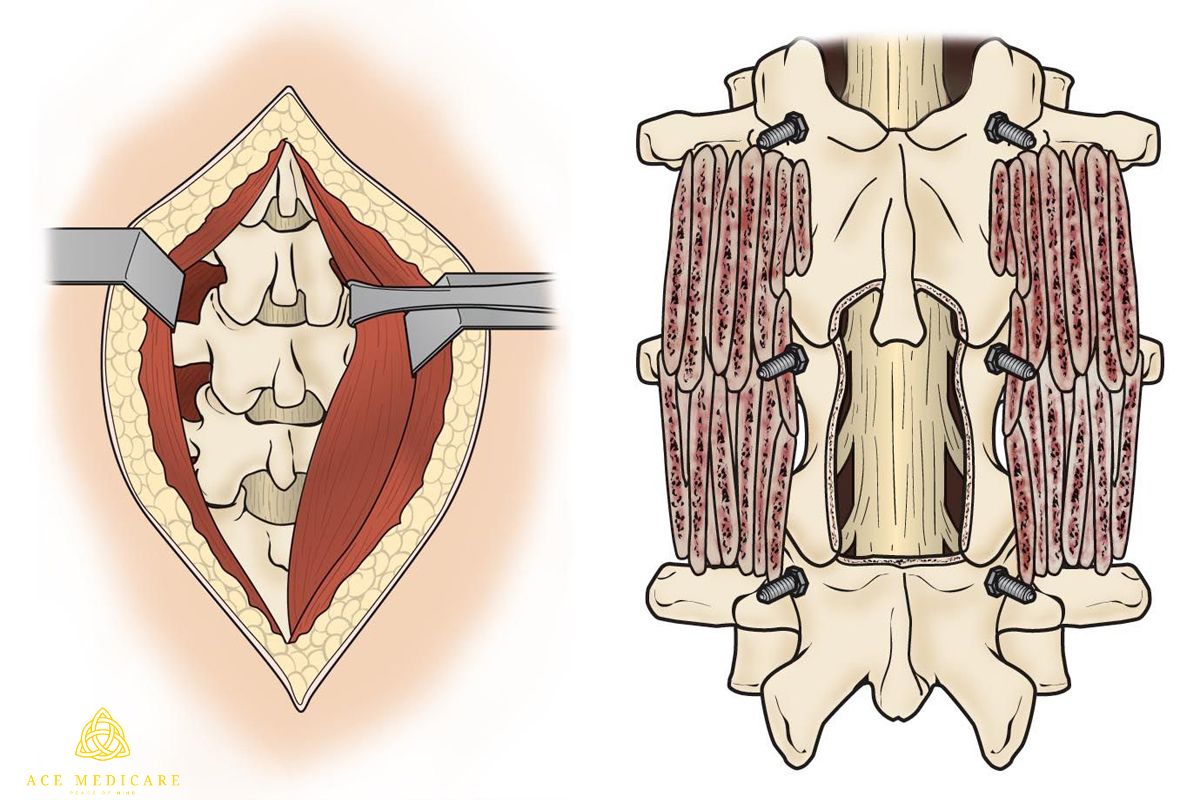
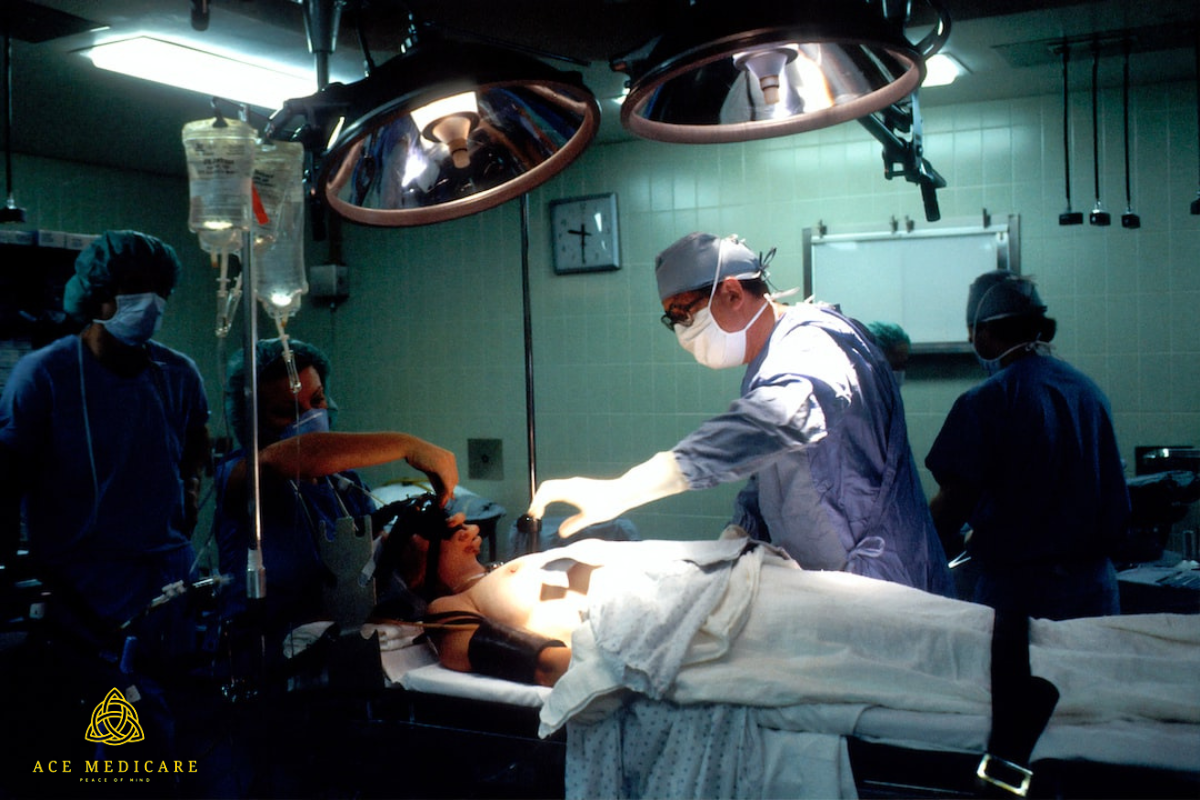
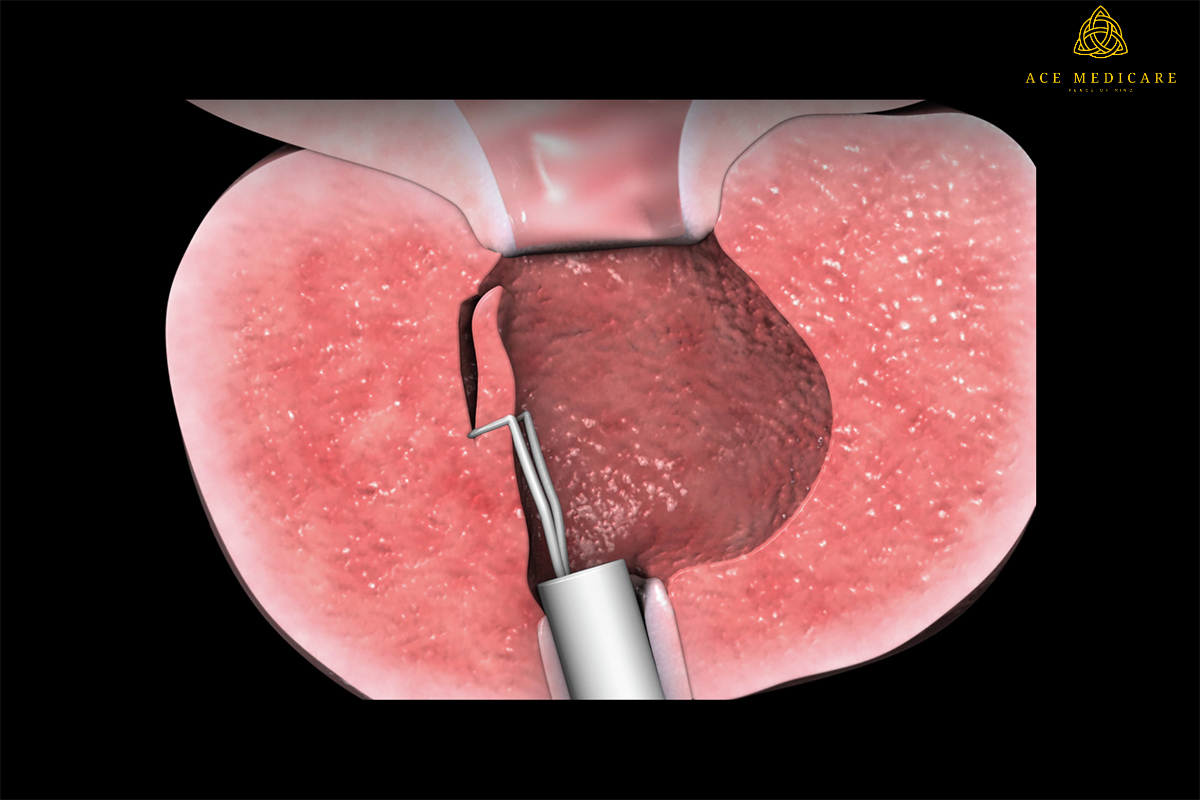
5. The Surgical Dance: Performing the Lung Transplant Procedure:
The actual lung transplant surgery is a carefully choreographed dance performed by skilled surgeons. Depending on the type of transplant, one or both lungs are replaced. Surgeons connect the new lungs to the recipient's blood vessels and airways with precision. The success of the surgery relies on the expertise and coordination of the surgical team.
6. Post-Transplant Recovery: Navigating the Early Challenges:
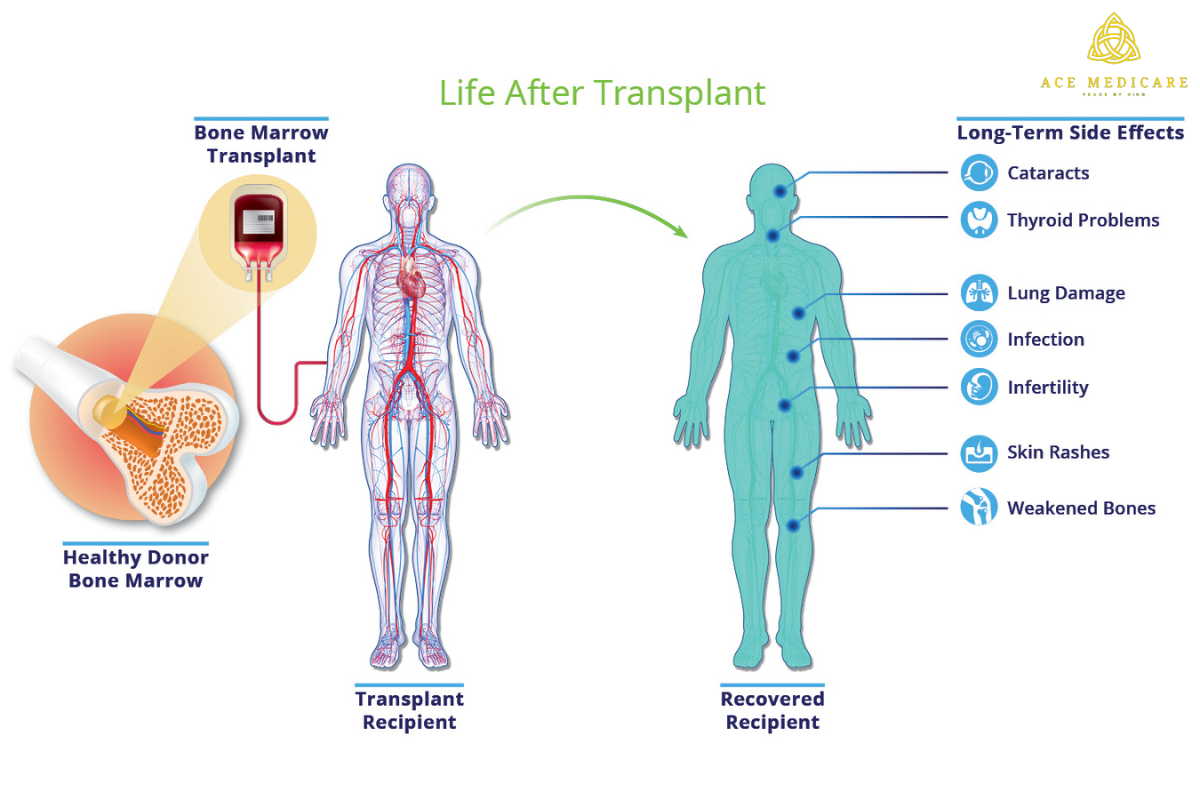
Recovery after a lung transplant involves an initial hospital stay of several weeks. During this period, recipients navigate challenges like pain management, monitoring for complications, and the initiation of immunosuppressive medications. The early post-transplant phase sets the stage for the recipient's long-term well-being.
7. Immunosuppressive Medications: Safeguarding the Gifted Lungs:
Immunosuppressive medications are prescribed post-transplant to prevent rejection. Adherence to this medication regimen is crucial, striking a balance between preventing rejection and minimizing the risk of infections and other complications. These medications are the guardians of the gifted lungs, ensuring their longevity.
8. Follow-Up Care and Monitoring: A Lifelong Partnership:
Lifelong follow-up care is essential for lung transplant recipients. Regular appointments, including lung function tests, imaging studies, and medication adjustments, are part of the ongoing monitoring process. The relationship with the transplant team, which may include pulmonologists and transplant coordinators, becomes an enduring partnership in the recipient's journey.
9. Potential Complications and Rejection: Navigating Challenges:
While lung transplants can be successful, there are potential complications, with rejection being a primary concern. Acute rejection occurs when the immune system perceives the transplanted lungs as foreign and attacks them. Recipients must remain vigilant for signs of rejection and adhere to medical recommendations to minimize these risks.
10. Quality of Life After a Lung Transplant: Breathing Freely Again:
A successful lung transplant often translates to a significantly improved quality of life. Recipients experience enhanced breathing, increased energy levels, and a return to activities that were once challenging. Despite the ongoing commitment to medical care, the chance at a renewed and active life is the ultimate reward for those who undergo a lung transplant.
Conclusion: A Symphony of Hope and Healing:
A lung transplant is more than a medical procedure; it's a symphony of hope and healing. From the initial diagnosis of end-stage lung disease to the intricacies of the transplant process and the ongoing commitment to post-transplant care, this guide provides a step-by-step journey through the transformative experience of a lung transplant. It embodies the resilience of the human spirit and the strides in medical science that continue to pave the way for a brighter future for individuals facing severe lung conditions. Trust Ace Medicare doctors for expert guidance and personalized support on your transformative journey.





.png)





.png)






.png)























.png)






































.png)























.png)
.png)





.png)































.png)




.png)





.png)












.png)






.png)