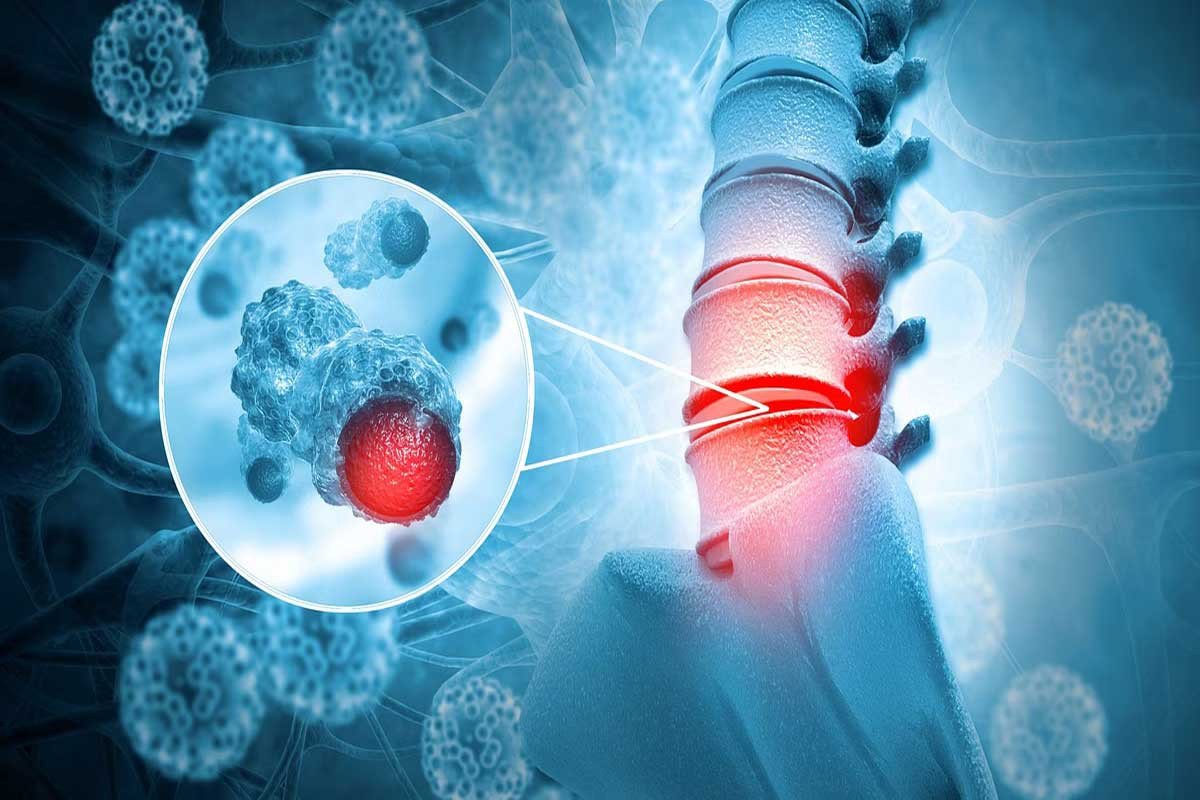
Spine Surgery with Minimal Invasive Techniques
The purpose of minimally invasive spine (MIS) surgery is to stabilise the vertebral bones and spinal joints and/or relieve pressure on the spinal nerves, which is typically caused by disorders such as spinal instability, bone spurs, ruptured discs, scoliosis, or spinal tumours.
Minimally invasive spine surgery can be faster, safer, and require less recovery time than open spine surgery. Because there is less stress to the muscles and soft tissues (in comparison to open treatments),
The potential benefits are as follows:
- Smaller skin incisions (as little as a few millimetres) produce better cosmetic benefits.
- Surgery results in less blood loss.
- Reduced risk of muscle damage because less or no muscle cutting is necessary Reduced risk of infection and postoperative discomfort
- Surgery recovery time is reduced, and rehabilitation is reduced.
- Reduced dependency on pain medicines following surgery
- Furthermore, certain MIS surgeries are conducted as outpatient procedures with only local anaesthesia, reducing the risk of an unfavourable reaction to general anaesthesia.
As with every surgical operation, no matter how minor, there are dangers involved.
These hazards include, but are not limited to:
- Possible anaesthetic adverse reaction
- During the surgery, there was unexpected blood loss.
- Localised infections, regardless of the size of the incision region
- And, while it is uncommon, there is always a potential that the initial MIS surgery would fail, necessitating either a second procedure or full open surgery.
MIS Procedures Used to Treat Conditions
- Degenerative disc disease is a type of disc disease.
- Disc herniation
- Spinal stenosis in the lumbar region
- Scoliosis is a type of spinal deformity.
- Infections of the spine
- Spondylolisthesis is a type of spinal instability.
- Compression fractures of the vertebrae
- Tumours in the spine
What is Minimally Invasive Spine Surgery?
Because the spinal nerves, vertebrae, and discs are positioned deep within the body, any strategy to gaining access to the spinal area necessitates the removal of muscle tissue. In general, this is made easier by making small incisions and guiding equipment and/or microscopic video cameras through them. Lasers are rarely employed in MIS operations, contrary to popular assumption.
A variety of techniques can be utilised to reduce trauma during MIS surgery. Here are some of the more frequent strategies.
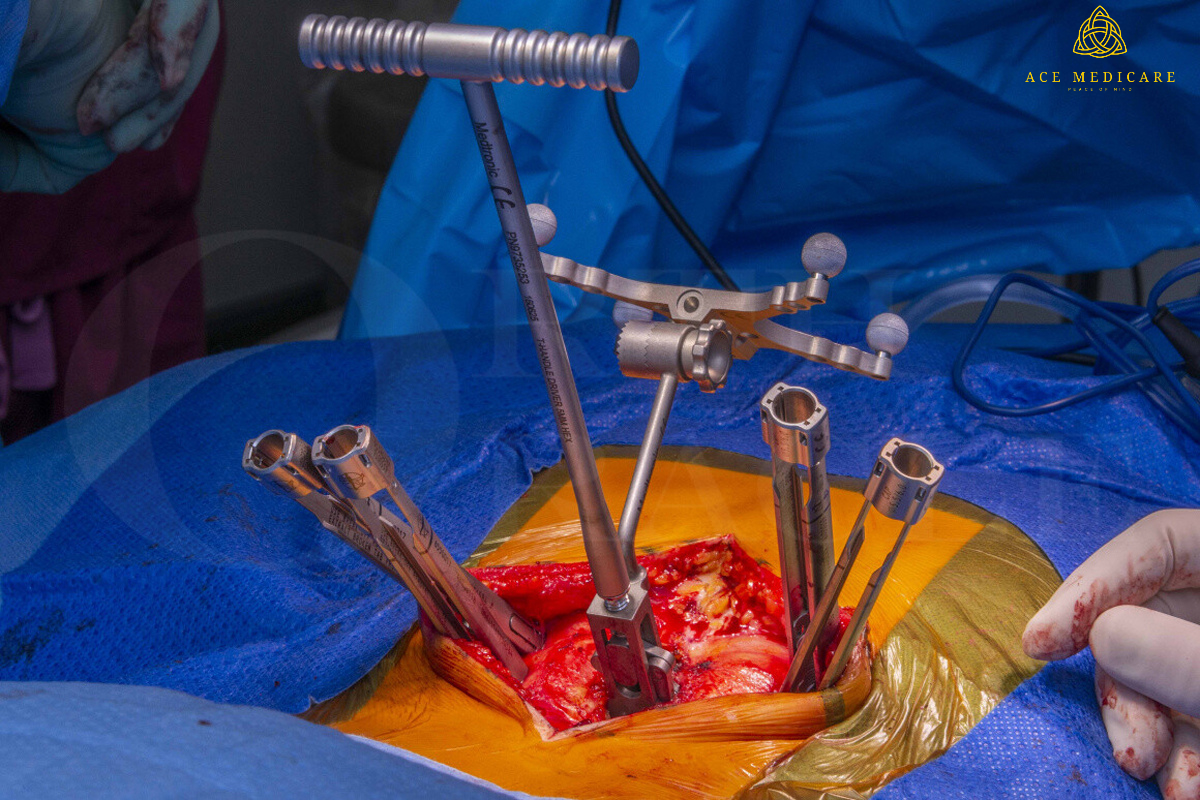
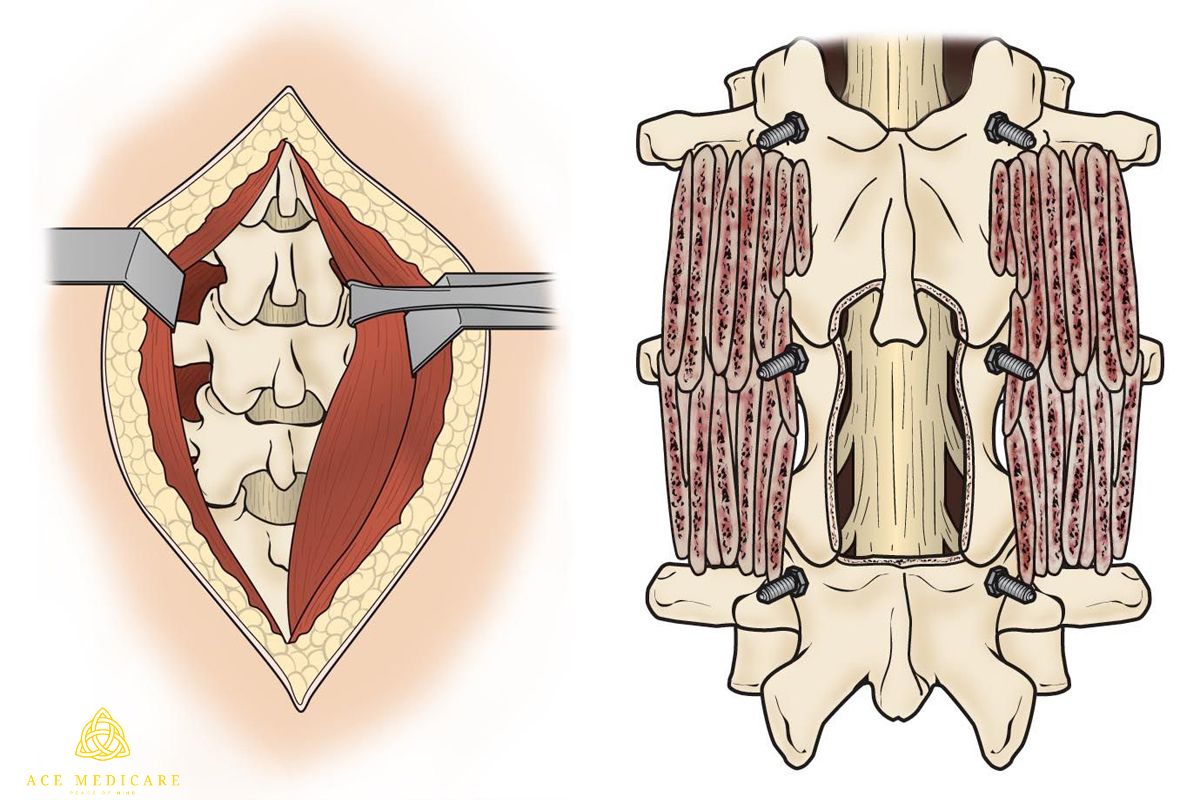
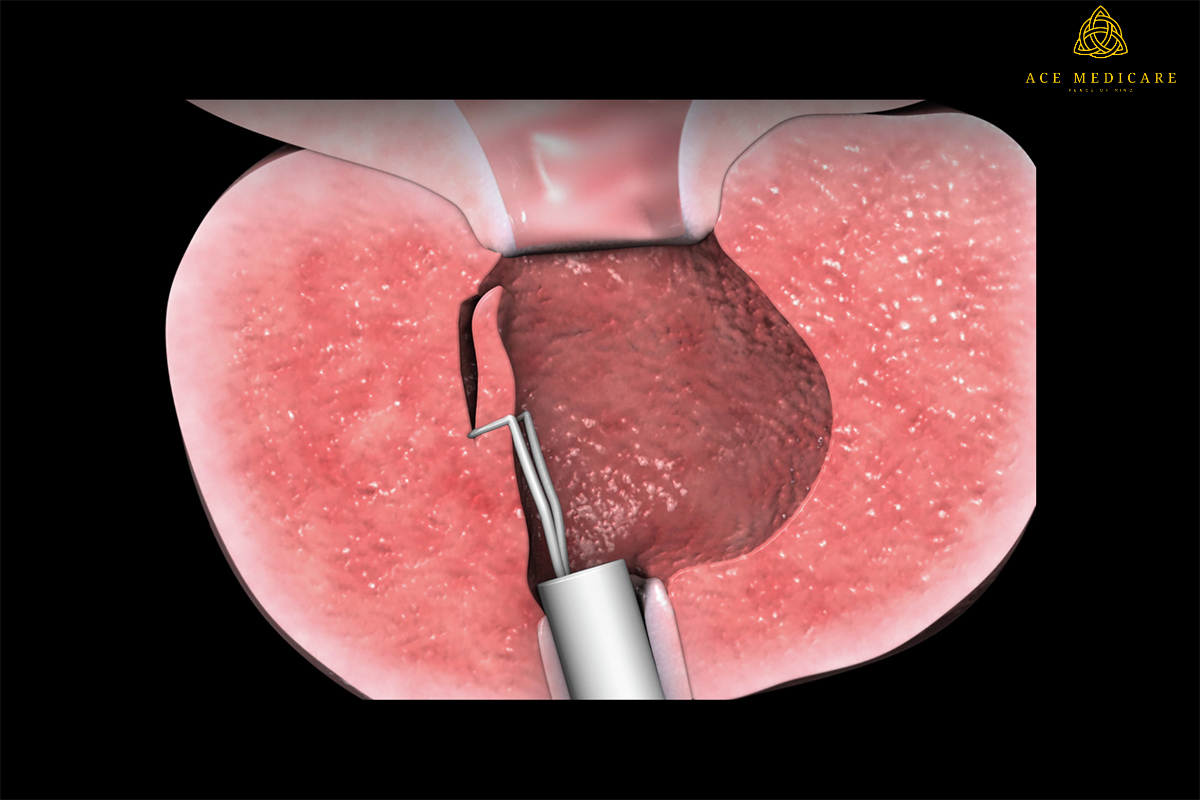
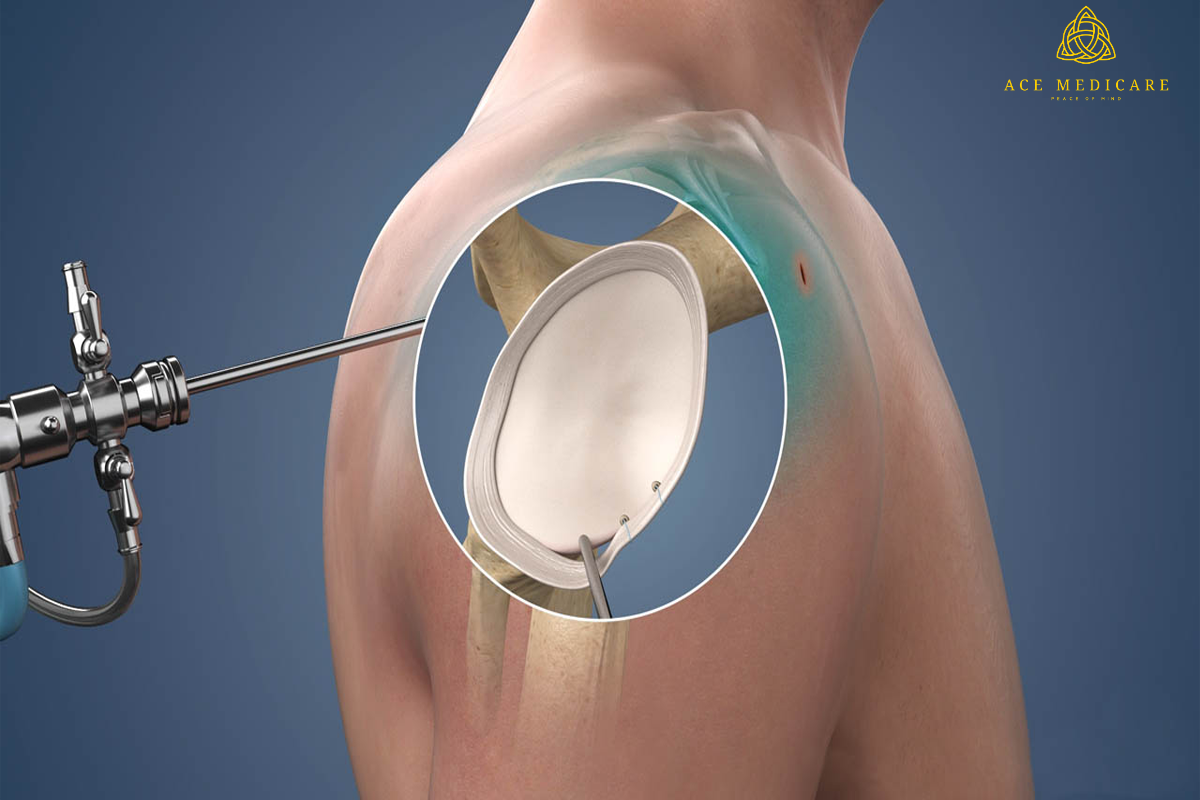
Making Use of a Tubular Retractor
Rather than cutting directly through the muscles, this approach requires progressive dilatation of the soft tissues. The surgeon used tubes to keep the muscles out of the way.works via the incision without exposing the area too much. When using a minimum access method, the surgeon may also use an endoscope or microscope directed down the tube to assist with the surgery. When the treatment is finished, the tubular retractor is withdrawn, allowing the dilated tissues to heal. Incisions might be tiny depending on the extent and type of surgery required.
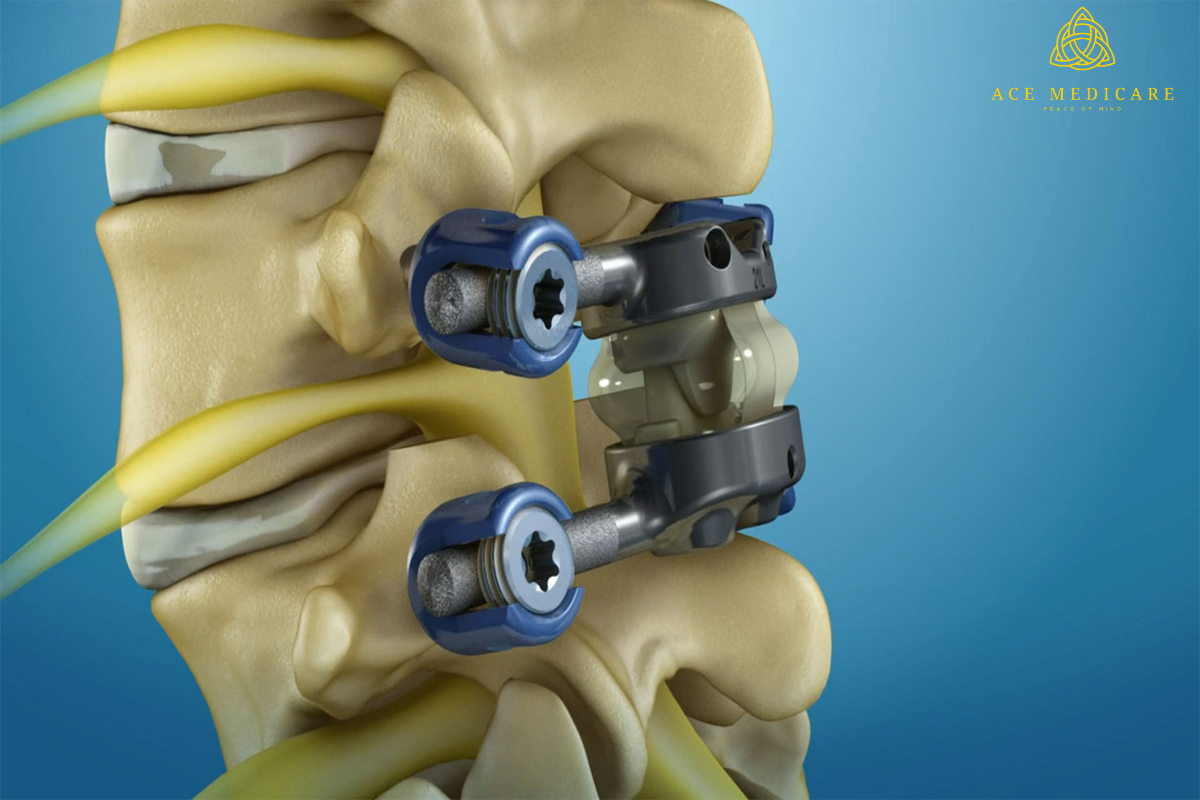
Screw and rod insertion through the skin
Depending on the patient's condition, equipment such as rods and screws may be required to stabilise the spine or immobilise the spine to facilitate spinal bone fusion. Traditional screw placement methods necessitate substantial excision of muscle and other tissues from the spine's surface.
Percutaneous (meaning "through the skin") implantation, on the other hand, often entails introducing rods and screws through small skin incisions without damaging or dissecting the underlying muscle. Guidewires are implanted through the skin and into the spinal vertebrae along the desired screw pathways using x-ray pictures. The screws are then positioned over the guidewires and follow the wires' course. These Screws have temporary extenders that extend outside the skin and are removed after guiding rod passage to join and fasten the screws. Spinal instrumentation is being implanted more safely and accurately because to the use of spinal navigation and robots.
Procedure Specifications
How should I get ready for spine surgery?
To get ready for spine surgery, do the following:
- If you smoke, you should stop. Request assistance from your service provider. There are drugs and programmes available to assist you in quitting.
- Exercise often to maintain your body and muscles in condition and to reduce recuperation time.
- Make sure you and your surgical team go over all of the products you use a few weeks before your operation. Non-essential drugs and herbal therapies may need to be discontinued. These may interact with anaesthetics or other drugs.
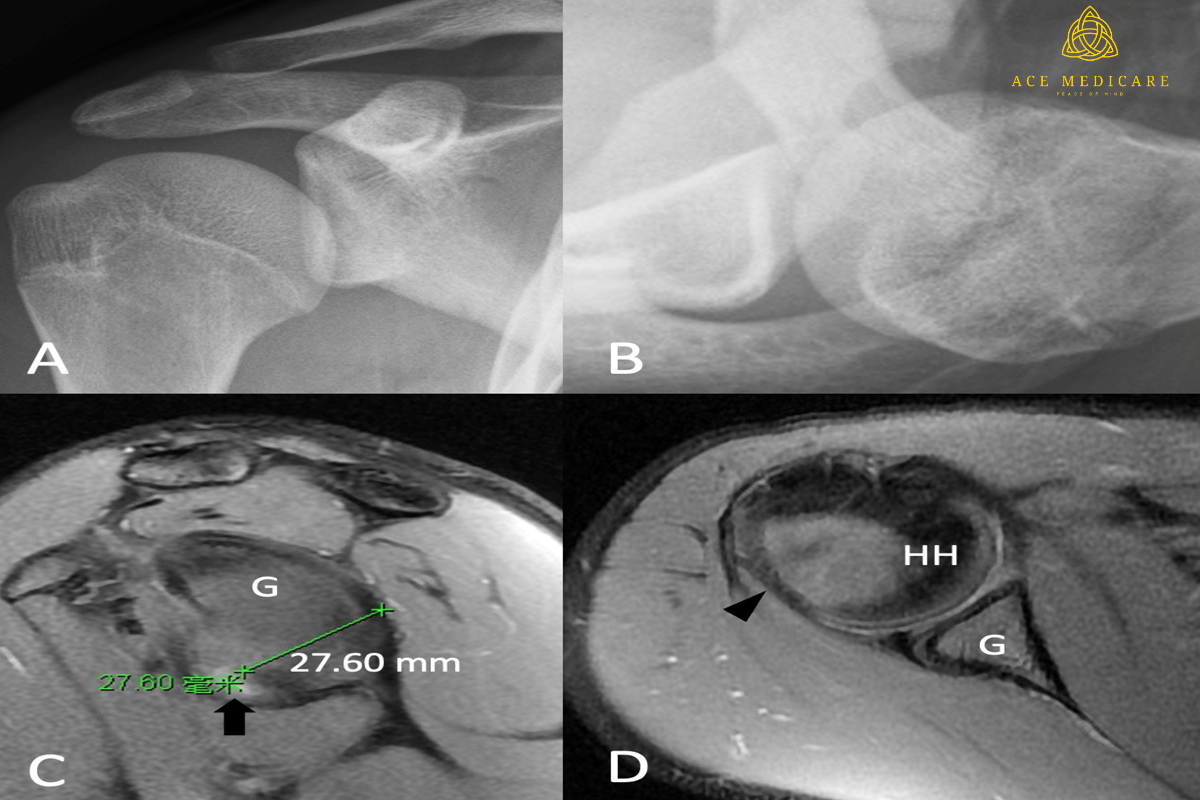
- X-rays or magnetic resonance imaging (MRI) of your spine will be ordered by your surgeon. Antibiotics may be prescribed before and after your procedure. Antibiotics are beneficial. Avoid infection. Your doctor will inform you what you may and cannot eat or drink the night before surgery.
What is the procedure for minimally invasive spine surgery through the Ace medicare?
Anaesthesia will be administered to you. Regional anaesthesia (numbing a section of your spine) or general anaesthesia (sleeping during your procedure) are also options.
There are various less invasive procedures available. They all have one thing in common: your surgeon makes one or more small incisions through your skin — through your back, chest, or abdomen – rather than one lengthy incision.
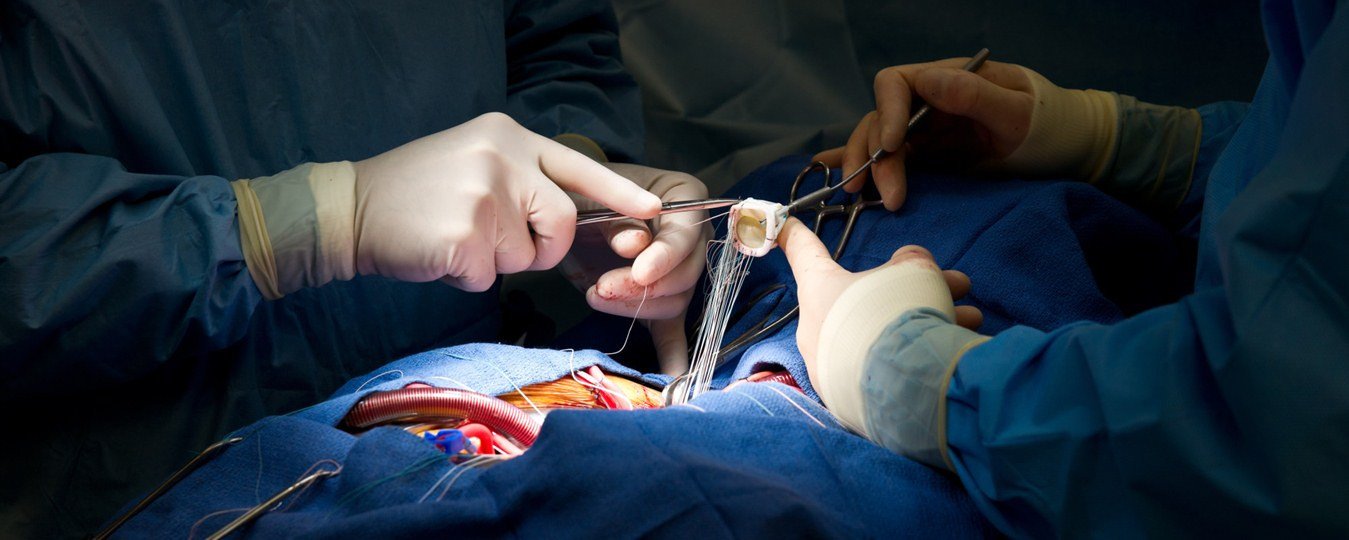
Your surgeon may use a fluoroscope or an endoscope to identify where to make incisions. A fluoroscope is a portable X-ray machine that offers images of your spine in real time during surgery. A narrow, telescope-like instrument is an endoscope. It is linked to a tiny video camera the size of a dime, which projects an interior picture of your spine onto television screens in the operating room. Small surgical instruments are passed through the endoscope or additional half-inch incisions where tubular retractors have been implanted.
Tubular retractors are hollow, thin tubes. Retractors generate little work tunnels from the hole in your skin to the targeted spot on your spine. One or more retractors are used to insert instruments. These retractors are also used to extract spinal bone and tissue removed during surgery. During surgery, tubular retractors keep your muscles away from the surgical site. When you remove the retractors, your muscles return to their previous place.
Following surgery, your It is linked to a tiny video camera the size of a dime, which projects an interior picture of your spine onto television screens in the operating room. Small surgical instruments are passed through the endoscope or additional half-inch incisions where tubular retractors have been implanted.
Tubular retractors are hollow, thin tubes. Retractors generate little work tunnels from the hole in your skin to the targeted spot on your spine. One or more retractors are used to insert instruments. These retractors are also used to extract spinal bone and tissue removed during spine surgery. During surgery, tubular retractors keep your muscles away from the surgical site. When you remove the retractors, your muscles return to their previous place.
Following surgery, your Sutures (stitches), glue, or staples are used to close incisions, which are then wrapped with surgical tape or tiny bandages.





.png)





.png)






.png)























.png)






































.png)























.png)
.png)





.png)































.png)




.png)





.png)












.png)






.png)